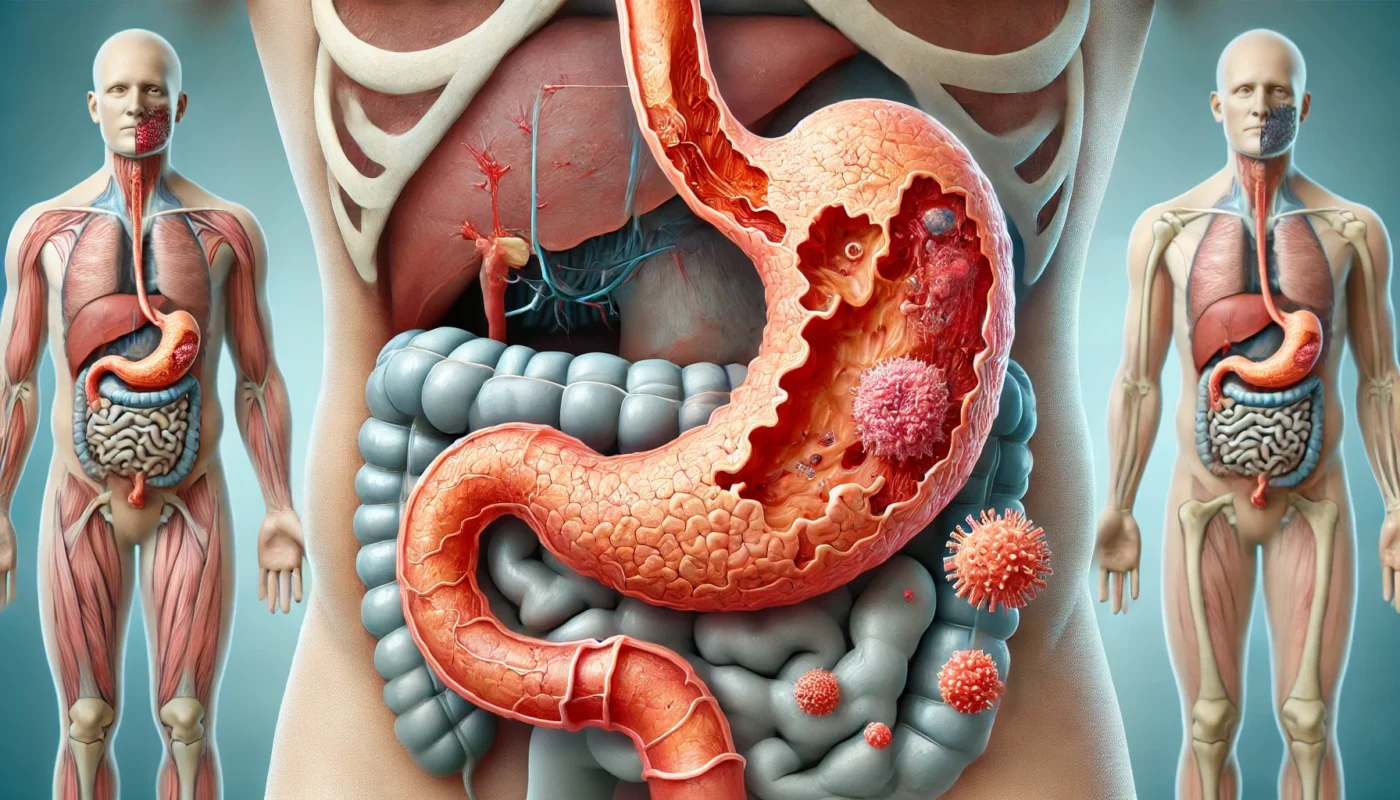
Autoimmune gastritis, also known as chronic atrophic autoimmune gastritis, is characterized by the immune system’s attack on the stomach’s parietal cells. These cells are responsible for producing hydrochloric acid and intrinsic factor, essential for vitamin B12 absorption. The destruction of these cells leads to a cascade of digestive issues, often resulting in vitamin B12 deficiency and, over time, can cause a form of anemia known as pernicious anemia.
The Role of Parietal Cells
Parietal cells play a crucial role in maintaining the stomach’s acidity, which is vital for digestion and nutrient absorption. When these cells are damaged, the stomach’s ability to break down food and absorb nutrients is impaired. This impairment can lead to several digestive complications, which may manifest as a variety of gastrointestinal symptoms.
Intrinsic Factor and Vitamin B12 Absorption
Intrinsic factor is a protein secreted by parietal cells that binds to vitamin B12, facilitating its absorption in the small intestine. Without adequate intrinsic factor, vitamin B12 absorption is severely compromised, leading to deficiencies that can have widespread effects on the body. This deficiency is particularly concerning because vitamin B12 is essential for nerve function and the production of red blood cells.
Progression to Pernicious Anemia
If autoimmune gastritis is left untreated, the persistent vitamin B12 deficiency can progress to pernicious anemia. This condition is characterized by the production of abnormally large and dysfunctional red blood cells, which can lead to severe fatigue, weakness, and other systemic symptoms. Early diagnosis and intervention are crucial to prevent this progression and to manage the associated symptoms effectively.
You May Also Like: Exploring the Irish Autoimmune Diet Benefits
Symptoms of Autoimmune Gastritis
Recognizing the symptoms of autoimmune gastritis is crucial for early diagnosis and management. The symptoms can be subtle at first but may progress over time. They include:
Digestive Symptoms
Abdominal Pain and Bloating
Abdominal pain and bloating are common complaints among sufferers, often mistaken for general indigestion or irritable bowel syndrome. These symptoms may fluctuate in intensity and can be exacerbated by dietary choices or stress. Understanding the specific triggers that worsen these symptoms can be beneficial for managing the condition effectively.
Nausea and Vomiting
Nausea and vomiting can be intermittent and vary in intensity, often occurring after meals. These symptoms may be mistaken for a stomach virus or food intolerance, delaying proper diagnosis. Keeping a symptom diary can help identify patterns and aid healthcare providers in diagnosing the condition accurately.
Diarrhea
Diarrhea is a frequent symptom in autoimmune gastrointestinal diseases, often exacerbated by dietary triggers. The disruption of normal digestive processes can lead to malabsorption, further complicating the nutritional deficiencies already present in autoimmune gastritis. Identifying and avoiding specific food triggers can help manage this symptom.
Systemic Symptoms
Fatigue
Fatigue is a common systemic symptom, resulting from anemia due to vitamin B12 deficiency. This type of fatigue is often persistent and can interfere with daily activities and quality of life. Addressing the underlying vitamin B12 deficiency through supplementation can significantly improve energy levels.
Neurological Issues
Prolonged vitamin B12 deficiency can lead to neurological issues such as tingling, numbness, or cognitive disturbances. These symptoms result from the vitamin’s crucial role in maintaining nerve health. Early recognition and treatment of vitamin B12 deficiency are essential to prevent permanent neurological damage.
Skin Changes
Skin changes, including pale or jaundiced skin, can occur due to underlying anemia. These changes are often accompanied by other symptoms such as dizziness or shortness of breath. Monitoring skin color and other signs of anemia can help track the effectiveness of treatment interventions.
Causes and Risk Factors
Genetic Predisposition
Familial Links
While no direct hereditary link has been fully established, a genetic predisposition may exist, particularly if there is a family history of autoimmune disorders. Understanding family medical history can provide valuable insights into potential risks and inform proactive health measures.
Autoimmune Disorder Associations
Autoimmune gastritis is often associated with other autoimmune disorders, such as type 1 diabetes or thyroid disease. Individuals with these conditions may have an increased risk of developing autoimmune gastritis, highlighting the importance of regular monitoring and early intervention.
Genetic Markers
Research into specific genetic markers associated with autoimmune gastritis is ongoing. Identifying these markers could lead to improved screening and personalized treatment strategies, offering hope for better management of the condition.
Environmental Factors
Dietary Influences
Diet plays a significant role in the onset and progression of autoimmune gastritis. Certain foods may trigger or exacerbate symptoms, while a balanced diet can support overall digestive health. Identifying and avoiding dietary triggers is a key component of managing the condition.
Lifestyle and Stress
Lifestyle factors, including stress, can impact the development and severity of autoimmune gastritis. Stress management techniques such as yoga, meditation, or regular exercise can help mitigate the effects of stress on the digestive system.
Infectious Agents
Exposure to certain infections, such as Helicobacter pylori, has been linked to the development of autoimmune gastritis. Ongoing research aims to clarify the role of infections in triggering or exacerbating the condition, potentially leading to new prevention and treatment strategies.
Diagnosis of Autoimmune Gastritis
Diagnosing autoimmune gastritis typically involves a combination of approaches:
Blood Tests
Blood tests are essential for checking for antibodies against parietal cells and intrinsic factor. These tests also measure vitamin B12 levels, providing insights into the extent of deficiency. Regular monitoring through blood tests helps track the progression of the disease and the effectiveness of treatments.
Endoscopy
Endoscopy allows for a visual inspection of the stomach lining for signs of atrophy, providing crucial information about the extent of damage. During the procedure, biopsy samples can be taken for further analysis, offering a more comprehensive understanding of the condition.
Gastric Biopsy
A gastric biopsy provides a definitive diagnosis by revealing characteristic changes in stomach tissue. This procedure helps confirm the presence of autoimmune gastritis and guides the development of an effective treatment plan. Combining biopsy results with other diagnostic tools ensures a comprehensive approach to diagnosis.

Treatment and Management Strategies
Managing autoimmune gastritis involves addressing both the symptoms and the underlying cause. Here are some strategies:
Vitamin B12 Supplementation
Injection Therapy
Since vitamin B12 deficiency is a hallmark of autoimmune gastritis, regular B12 injections are often necessary. This method ensures direct absorption into the bloodstream, bypassing issues with intrinsic factor production.
High-Dose Oral Supplements
High-dose oral supplements provide an alternative to injections, though absorption can be less predictable. Monitoring vitamin B12 levels regularly can help determine the most effective supplementation strategy for each individual.
Monitoring and Adjustments
Ongoing monitoring of vitamin B12 levels is crucial to ensure adequate supplementation. Adjustments to dosage or frequency may be needed based on blood test results and symptom changes.
Dietary Modifications
Nutrient-Rich Diet
Adopting a diet rich in nutrients and low in irritants can help manage symptoms. Foods high in folate, iron, and other essential nutrients support overall health and can mitigate the effects of vitamin B12 deficiency.
Avoiding Trigger Foods
Avoiding foods that exacerbate symptoms, such as spicy or acidic items, can provide relief. Identifying personal food triggers through a food diary or elimination diet can help tailor dietary choices.
Professional Guidance
Consulting with a dietitian or nutritionist can provide personalized dietary recommendations. Professional guidance ensures a balanced approach to diet, supporting digestive health and overall well-being.
Medical Interventions
Proton Pump Inhibitors (PPIs)
Proton pump inhibitors (PPIs) may be prescribed to reduce stomach acid production, providing symptomatic relief. While they do not address the underlying cause, they can improve quality of life by alleviating uncomfortable symptoms.
Anemia Treatments
In cases of significant anemia, additional treatments such as iron supplements or blood transfusions may be necessary. Addressing anemia comprehensively involves monitoring blood levels and adjusting treatments as needed.
Regular Medical Check-Ups
Regular medical check-ups are essential for monitoring the progression of autoimmune gastritis and adjusting treatment plans. Ongoing communication with healthcare providers ensures that symptoms are managed effectively.
Holistic and Alternative Approaches
Some individuals find relief in holistic methods, such as:
Acupuncture
Acupuncture may help alleviate digestive symptoms and promote overall well-being. By targeting specific pressure points, acupuncture can reduce stress and improve digestive function.
Herbal Supplements
Herbal supplements like ginger and turmeric, known for their anti-inflammatory properties, could support digestive health. Incorporating these supplements into a daily routine may help reduce inflammation and improve symptom management.
Probiotics
Maintaining gut flora balance through probiotics might improve digestive function and mitigate symptoms. Probiotics support a healthy microbiome, which is crucial for overall digestive health.

Long-term Management and Lifestyle Adjustments
Living with autoimmune gastritis requires ongoing management to prevent complications and improve quality of life:
Regular Monitoring
Regular monitoring through routine blood tests helps track vitamin levels and adjust treatment accordingly. Staying informed about changes in health status empowers individuals to make proactive decisions about their care.
Mind-Body Practices
Mind-body practices such as yoga or meditation can help reduce symptom flares by managing stress. Incorporating these practices into daily life supports overall well-being and enhances the body’s resilience to stressors.
Patient Education
Understanding the condition and its implications empowers patients to make informed decisions about their health care. Engaging with educational resources and support groups can provide valuable insights and encouragement.
Building a Support Network
Building a support network of healthcare providers, family, and friends can offer emotional and practical support. Sharing experiences and learning from others can enhance coping strategies and improve quality of life.
Conclusion
Autoimmune gastritis is a chronic condition that requires a multifaceted approach to manage effectively. By combining traditional medical treatments with holistic strategies, individuals can achieve better control over their symptoms and improve their overall health and well-being. Whether you’re navigating this condition yourself or supporting someone who is, understanding the complexities of autoimmune gastritis is a vital step towards effective management.
By staying informed and proactive, you can optimize your digestive health and enhance your quality of life. Always consult with healthcare professionals to tailor a management plan that suits your specific needs. Through education, support, and personalized care, individuals with autoimmune gastritis can lead fulfilling lives.
Further Reading:
Autoimmune diseases in autoimmune atrophic gastritis
What to know about atrophic gastritis
Autoimmune Gastritis and Gastric Microbiota
autoimmune gastritis, vitamin B12 deficiency, dietary modifications, holistic health, probiotics, acupuncture, herbal supplements, digestive health, patient education, medical interventions, anemia treatments, lifestyle adjustments, nutrient-rich diet, stress management, support network, health monitoring
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.