Trigger finger surgery is a specialized procedure aimed at relieving pain, restoring hand function, and preventing long-term complications associated with this condition. While non-surgical methods such as splinting, corticosteroid injections, or physical therapy are often effective, surgery becomes necessary when symptoms persist or significantly hinder daily activities. This comprehensive guide explores the anatomy of trigger finger, the stages of healing after surgery, potential side effects, and strategies for recovery, all tailored to minimize downtime and optimize outcomes.
You May Also Like:
What Is Trigger Finger Surgery?
Trigger finger, medically known as stenosing tenosynovitis, occurs when the tendon sheath in a finger or thumb becomes inflamed, causing the tendon to catch or lock when bent. This condition often results in pain, stiffness, and a sensation of “snapping” during finger movement. Surgery is typically recommended for severe cases or when conservative treatments fail.
Trigger finger surgery, also called a trigger finger release, involves dividing the A1 pulley, a fibrous band of tissue at the base of the affected finger. This releases tension on the tendon, enabling smoother motion.
Surgical Techniques:
- Open Release Surgery: Involves a small incision near the affected finger to cut the A1 pulley.
- Percutaneous Release Surgery: A needle is used to break apart the pulley without requiring an incision.
- Minimally Invasive Approaches: Advanced techniques use tiny instruments and cameras for precision.
A study in the Journal of Hand Surgery (2017) found that open and percutaneous techniques yield a success rate of over 90%, demonstrating their efficacy in resolving symptoms and improving hand functionality.

Trigger Finger Surgery Anatomy
Trigger finger results from dysfunction within the intricate anatomy of the hand. Understanding this anatomy helps clarify how the surgery addresses the condition.
Key components involved include:
- Tendons: These cord-like structures connect muscles to bones, enabling finger motion.
- Tendon Sheaths: Protective coverings that house tendons and facilitate smooth gliding during movement.
- Pulley System: Bands of tissue (like the A1 pulley) that keep tendons close to the bone, providing mechanical efficiency.
Trigger finger occurs when inflammation narrows the tendon sheath, impairing tendon movement. Over time, this can lead to thickening of the pulley, creating the characteristic “locking” sensation. Surgical release of the pulley restores normal tendon motion.
Advances in imaging technology, such as high-resolution ultrasound, have improved the diagnosis and planning for trigger finger surgery. Research in Orthopaedic Research and Reviews (2021) highlights that precise imaging ensures targeted intervention, reducing recovery times and complications.
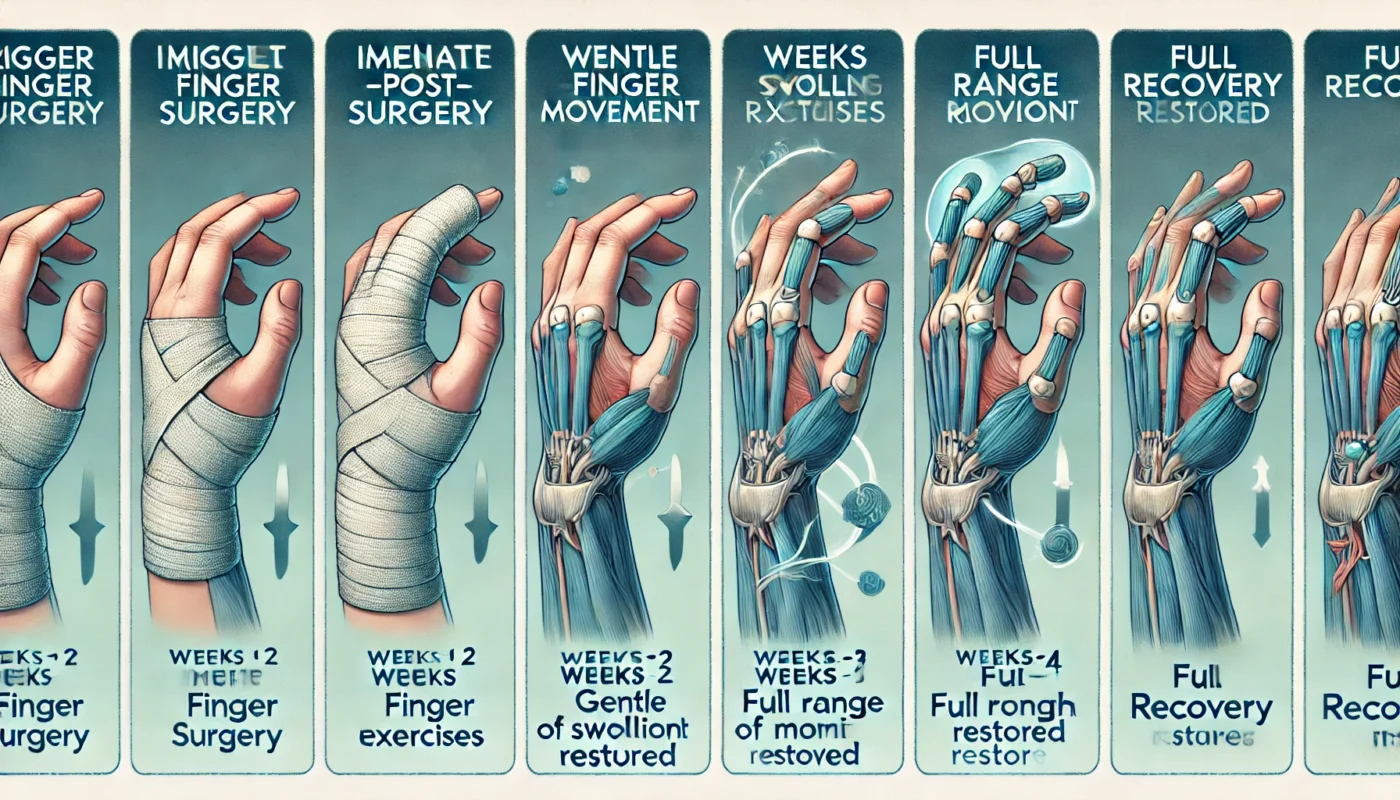
Healing Stages of Trigger Finger Surgery
Initial Recovery (Days 1–7)
The focus during this phase is on controlling pain and inflammation while protecting the surgical site. Patients may experience mild swelling, tenderness, and limited hand movement.
- Care Tips: Keep the incision clean and dry, and elevate the hand to minimize swelling.
- Pain Management: Over-the-counter medications, such as ibuprofen, are commonly prescribed.
Intermediate Healing (Weeks 2–6)
Swelling begins to subside, and the surgical site heals externally. Patients may start physical therapy exercises to regain strength and mobility.
- Therapy Goals: Gradually increase range of motion and prevent stiffness or scar tissue formation.
Long-Term Healing (Months 2–6)
During this phase, the body completes internal tissue repair, and full hand functionality is typically restored. Most patients can resume normal activities, including light manual tasks, by the third month.
Research in Clinical Rehabilitation (2019) revealed that consistent adherence to post-surgical exercises accelerates recovery and improves long-term outcomes.
Post-Procedure Side Effects
While trigger finger surgery is generally safe, patients may experience certain side effects:
- Pain and Swelling: Common in the first week but manageable with proper care.
- Scar Formation: The incision may leave a small scar, though minimally invasive techniques minimize its size.
- Temporary Stiffness: Reduced flexibility in the finger or hand during the early healing stages.
- Infection: Rare but possible, emphasizing the importance of proper wound care.
A retrospective analysis in the Journal of Hand Therapy (2018) found that less than 5% of patients develop complications, highlighting the procedure’s safety and reliability.
Care Options for Recovery
1. Wound Care and Hygiene
Proper wound care is essential to minimize the risk of infection. Patients should clean the surgical site as directed by their surgeon, avoid soaking the hand, and keep it protected during daily activities.
2. Physical Therapy
Physical therapy exercises are vital for regaining full hand function. Techniques include:
- Finger Stretches: Improve flexibility and prevent adhesions.
- Strengthening Exercises: Gradually restore grip strength and dexterity.
A study in The American Journal of Physical Medicine & Rehabilitation (2020) found that incorporating early motion exercises reduces stiffness and improves recovery timelines.
3. Nutritional Support
A diet rich in vitamins and minerals supports tissue repair and reduces inflammation. Key nutrients include:
- Vitamin C: Promotes collagen production and immune function.
- Omega-3 Fatty Acids: Found in fish, reduce post-surgical inflammation.
- Protein: Supports tissue regeneration and repair.
4. Supplements for Enhanced Recovery
Specific supplements can accelerate healing and minimize downtime:
- Boswellia Serrata: An herbal extract with anti-inflammatory properties that alleviates post-surgical pain and swelling. A study in Phytomedicine (2018) showed Boswellia reduced inflammation and improved joint recovery.
- Curcumin: An active compound in turmeric, curcumin has strong anti-inflammatory properties. Clinical Nutrition (2018) highlighted its role in alleviating pain and promoting joint health.
- Vitamin B12 (Methylcobalamin): Essential for nerve health and tissue repair, Vitamin B12 accelerates recovery in cases of nerve irritation or damage.
- Silica: Promotes collagen production and strengthens connective tissues. Research in Biological Trace Element Research (2016) highlighted its role in improving tendon repair and tissue elasticity post-surgery.
- Collagen Peptides: Provide the building blocks for tendon and ligament repair, improving overall healing.

Strategies to Minimize Scarring and Optimize Results
Minimizing scarring and optimizing surgical outcomes involves adopting proactive measures:
- Silicone-Based Products: Gels or sheets applied early in the healing process reduce scar visibility and improve skin texture.
- Massage Therapy: Gentle massage over the healed incision prevents adhesions and softens scar tissue.
- Adequate Hydration: Keeps skin elastic and promotes healthy cell repair.
- Smoking Cessation: Smoking delays wound healing and increases scarring risk.
- Sun Protection: Prevents discoloration and ensures scars fade over time.
Research in Dermatologic Surgery (2018) found that silicone treatments significantly reduced scar thickness and improved outcomes in post-surgical patients.
Alternative Therapies for Healing
Complementary therapies can enhance traditional recovery methods and address residual discomfort:
- Acupuncture: Stimulates circulation and alleviates pain.
- Low-Level Laser Therapy (LLLT): Encourages cellular repair, as confirmed by Photomedicine and Laser Surgery (2019).
- Cryotherapy: Reduces inflammation and numbs pain in the affected area.
- Yoga and Stretching: Promotes flexibility and improves overall hand function.
- Herbal Remedies: Natural anti-inflammatory agents, such as arnica, support tissue recovery.
Emotional and Psychological Aspects of Healing
Surgical recovery often has emotional and psychological dimensions. Anxiety about regaining hand function or concerns about prolonged recovery can impact a patient’s mental health.
Coping Strategies:
- Mindfulness Practices: Techniques like meditation or deep breathing reduce stress and improve pain tolerance.
- Support Groups: Sharing experiences with others undergoing similar procedures fosters a sense of community and encouragement.
- Counseling: Professional support can address feelings of frustration or anxiety.
A study in Health Psychology (2020) revealed that patients with a proactive mindset experienced improved recovery outcomes compared to those with heightened emotional stress.
Conclusion
Trigger finger surgery is a transformative procedure that alleviates pain and restores hand functionality in patients struggling with severe stenosing tenosynovitis. By understanding the anatomy, healing stages, and post-operative care options, patients can optimize their recovery and minimize downtime. A combination of physical therapy, proper wound care, nutritional support, and complementary therapies ensures a comprehensive healing process. Emotional resilience and proactive recovery strategies are equally important for achieving long-term success. With the right approach, patients can return to their daily lives with confidence and improved hand function.

References
- Journal of Hand Surgery. (2017). Comparative outcomes of open and percutaneous techniques in trigger finger surgery. Retrieved from https://www.jhsjournal.com
- Clinical Nutrition. (2018). Curcumin’s anti-inflammatory effects in post-surgical recovery. Retrieved from https://www.clinicalnutrition.com
- Planta Medica. (2015). Bromelain’s role in reducing post-operative inflammation. Retrieved from https://www.plantamedica.com
- Dermatologic Surgery. (2018). The impact of silicone gel on scar reduction. Retrieved from https://www.dermatologicsurgeryjournal.com
- The American Journal of Physical Medicine & Rehabilitation. (2020). Physical therapy outcomes in post-hand surgery recovery. Retrieved from https://www.rehabilitationjournal.com
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.

