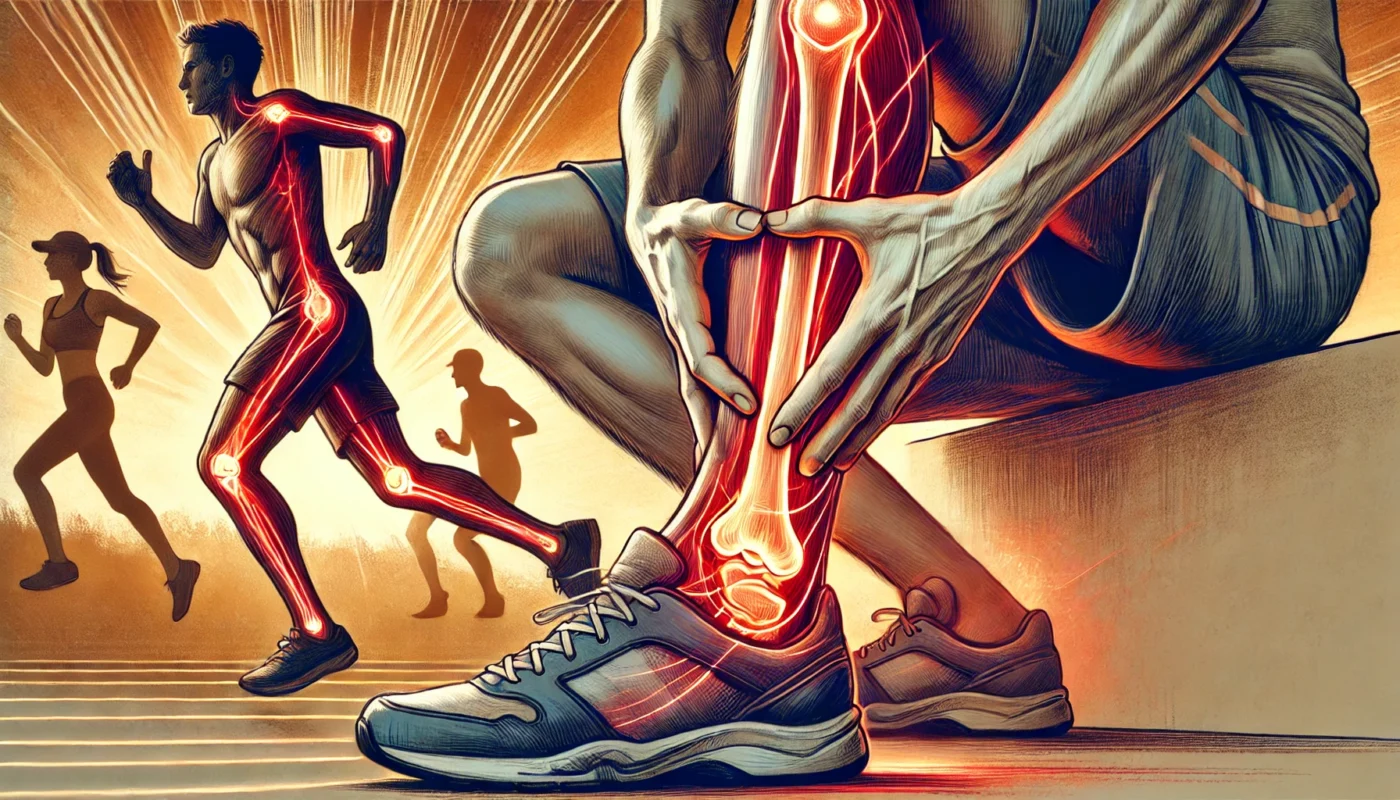
Shin splints, or medial tibial stress syndrome (MTSS), are a common condition affecting athletes, runners, and individuals engaged in repetitive impact activities. This article explores the key aspects of shin splints, including their symptoms, causes, treatment options, recovery strategies, and preventative measures. Additionally, we discuss nutritional supplementation that may support recovery by reducing inflammation and promoting tissue repair.
You May Also Like:
What Are Shin Splints?
Shin splints refer to pain along the inner edge of the tibia (shinbone) caused by inflammation of the muscles, tendons, and bone tissue in the lower leg. They are often associated with repetitive stress and overuse, particularly in activities involving running or jumping. Shin splints are not a single condition but rather a spectrum of injuries ranging from minor inflammation to stress fractures.
According to a study published in The American Journal of Sports Medicine in 2018, shin splints account for up to 15% of all running-related injuries, highlighting their prevalence among active populations.

Symptoms of Shin Splints
The symptoms of shin splints can vary in severity but typically include:
- Pain Along the Shinbone: A dull, aching pain that worsens during physical activity and may persist after exercise.
- Tenderness or Soreness: Sensitivity to touch along the inner edge of the shinbone.
- Mild Swelling: Localized swelling or puffiness in the lower leg.
- Pain with Activity: Increased discomfort during running, jumping, or similar activities.
- Stiffness: A feeling of tightness in the lower leg, particularly after waking up or resting.
These symptoms can interfere with athletic performance and daily activities if left untreated.
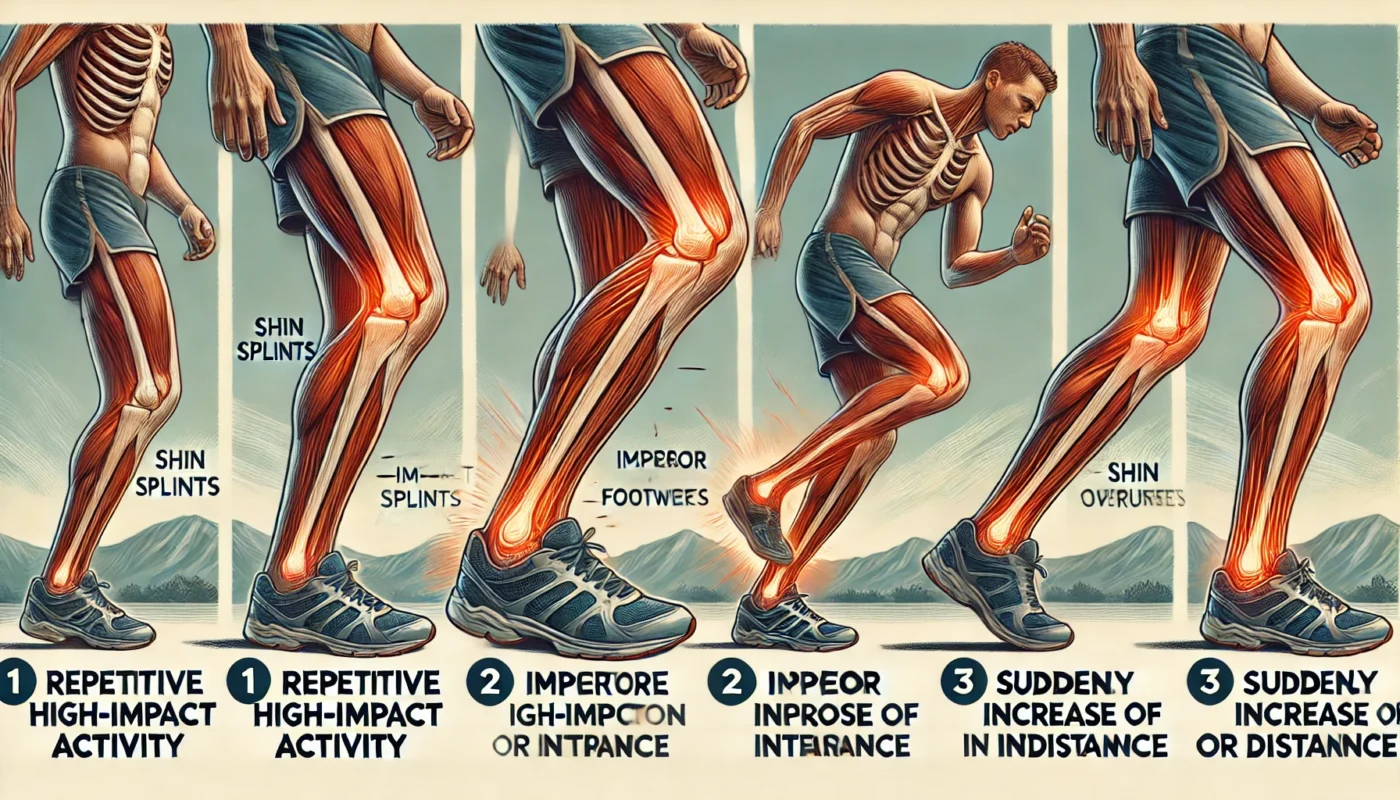
Causes of Shin Splints
Shin splints occur due to repetitive stress on the tibia and surrounding tissues. Common causes include:
- Overuse and Overtraining: Engaging in high-impact activities without adequate rest can overwhelm the body’s ability to recover. A 2020 study in Sports Health identified overtraining as the leading cause of shin splints in runners.
- Improper Footwear: Shoes lacking proper arch support or cushioning can exacerbate the impact on the lower legs. Research in The Journal of Foot and Ankle Research (2019) highlighted a strong correlation between inadequate footwear and the development of shin splints.
- Biomechanical Issues: Abnormal foot mechanics, such as flat feet or overpronation, can increase stress on the tibia and surrounding structures. A 2017 study in Clinical Biomechanics found that individuals with flat feet were 2.5 times more likely to develop shin splints.
- Sudden Increases in Activity: Rapidly increasing training intensity, duration, or frequency can strain the muscles and bones of the lower leg.
- Hard or Uneven Surfaces: Running on hard surfaces, such as concrete, or uneven terrain can increase impact forces, contributing to shin splints.
Treatment Options for Shin Splints Recovery
Effective treatment for shin splints focuses on relieving pain, reducing inflammation, and promoting healing. Common approaches include:
1. Rest
Rest is critical to allow the affected tissues to heal. Avoid high-impact activities that worsen symptoms and consider low-impact alternatives like swimming or cycling.
2. Ice Therapy
Applying ice packs to the affected area for 15–20 minutes, several times a day, can reduce inflammation and alleviate pain.
3. Compression and Elevation
Using a compression bandage can help minimize swelling, while elevating the leg above heart level reduces inflammation.
A physical therapist can provide exercises to strengthen the lower leg muscles, improve flexibility, and correct biomechanical issues. A study in The Journal of Sports Rehabilitation (2021) found that targeted exercises reduced shin splint recurrence rates by 35%.
5. Pain Relief
Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, can provide temporary relief. However, they should be used under the guidance of a healthcare professional.
6. Shockwave Therapy
Extracorporeal shockwave therapy (ESWT) has shown promise in treating chronic shin splints. A clinical trial in The Journal of Orthopaedic Research (2020) demonstrated that ESWT improved pain and function in patients with persistent shin splints.
7. Nutritional Support
Nutritional supplements can enhance recovery by reducing inflammation and promoting tissue repair. Effective options include:
- Bromelain: This pineapple-derived enzyme helps reduce swelling and pain. A 2018 trial in Alternative Medicine Review found bromelain effective for soft tissue injuries.
- Vitamin C: Essential for collagen synthesis and tissue repair. A randomized trial in Nutrients (2019) demonstrated enhanced healing in patients supplementing with vitamin C.
- Magnesium Glycinate: Magnesium plays a vital role in muscle relaxation and tissue repair. Research in Magnesium Research (2017) showed that magnesium supplementation improved recovery in athletes with muscle injuries.
- Glucosamine and Chondroitin: These compounds support joint and cartilage health, promoting recovery in stress-related injuries.
- Omega-3 Fatty Acids: Known for their anti-inflammatory effects, omega-3s can reduce pain and accelerate recovery. A 2020 study in Frontiers in Nutrition confirmed their benefits in managing musculoskeletal injuries.
- Turmeric: Curcumin, the active compound in turmeric, has potent anti-inflammatory properties. A 2016 study in The Journal of Medicinal Food reported reduced pain and inflammation in athletes supplementing with curcumin.

Steps for Possible Prevention of Shin Splints
Preventing shin splints involves addressing risk factors and adopting strategies to minimize stress on the lower legs. Key measures include:
1. Wear Proper Footwear
Choose shoes with adequate arch support, cushioning, and shock absorption. Replace worn-out shoes regularly to maintain optimal support.
2. Gradually Increase Activity
Avoid sudden increases in training intensity or duration. Follow the 10% rule, increasing activity levels by no more than 10% per week.
3. Strengthen Lower Leg Muscles
Strengthening exercises for the calves, tibialis anterior, and foot muscles can improve resilience to repetitive stress.
4. Warm-Up and Stretch
Incorporate dynamic warm-up routines and stretches for the calves, hamstrings, and Achilles tendons before engaging in high-impact activities.
5. Cross-Train
Alternate high-impact activities with low-impact options, such as swimming or cycling, to reduce repetitive strain on the tibia.
6. Use Orthotics
Custom orthotics or insoles can correct biomechanical issues and provide additional support.
7. Train on Softer Surfaces
Opt for grass, dirt trails, or rubberized tracks over hard surfaces to reduce impact forces on the legs.
Conclusion
Shin splints are a common overuse injury that can significantly impact athletic performance and daily activities. Understanding the symptoms, causes, and effective treatment strategies is essential for recovery. Rest, physical therapy, and nutritional supplementation, including turmeric, bromelain, magnesium glycinate, vitamin C, and omega-3 fatty acids, can support healing and reduce inflammation.
Implementing preventative measures, such as proper footwear, gradual training progression, and strengthening exercises, can help reduce the risk of shin splints. By taking proactive steps, individuals can maintain lower leg health and continue engaging in physical activities without interruption.

References
- Omega-3 Fatty Acid Supplementation on Post-Exercise Inflammation, Muscle Damage, Oxidative Response, and Sports Performance in Physically Healthy Adults—A Systematic Review of Randomized Controlled Trials. Retrieved from: https://pmc.ncbi.nlm.nih.gov/articles/PMC11243702/
- Acute protease supplementation effects on muscle damage and recovery across consecutive days of cycle racing. Retrieved from: https://pubmed.ncbi.nlm.nih.gov/25604346/
- Running Injury Paradigms and Their Influence on Footwear Design Features and Runner Assessment Methods: A Focused Review to Advance Evidence-Based Practice for Running Medicine Clinicians. Retrieved from: https://pmc.ncbi.nlm.nih.gov/articles/PMC8959543/
- Risk Factors for Medial Tibial Stress Syndrome in Active Individuals: An Evidence-Based Review. Retrieved from: https://pmc.ncbi.nlm.nih.gov/articles/PMC5264561/
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.