Scarring is an inevitable part of the body’s natural healing process. Whether it’s a small cut, a surgical incision, or a significant injury, scars form as the skin repairs itself. Understanding the factors that affect scar healing duration can help you manage expectations and take proactive steps to improve healing outcomes.
In this article, we’ll explore the various factors influencing how long scars stay red, the overall scar healing timeline, and strategies to minimize old scars. We’ll also delve into different types of scars and whether they can fade or disappear over time. Let’s dive in.
You may also like: Key Factors in Proliferative Wound Healing
What Determines How Long a Scar Stays Red?
The redness of a scar is primarily due to increased blood flow to the affected area as the body works to repair damaged tissue. This redness is a normal part of the healing process and can last anywhere from a few weeks to several months, depending on several factors.
Nature of the Injury
The severity and depth of the wound significantly impact how long a scar stays red. Deeper wounds typically result in more pronounced scarring and extended redness. Surgical scars, for example, may remain red for an extended period due to the precise nature of the incision and the body’s robust healing response. Additionally, wounds that involve extensive tissue damage or loss may take longer to heal, as the body must work harder to regenerate and repair the affected area.
In contrast, superficial wounds, such as minor cuts or abrasions, often heal more quickly and with less pronounced redness. The body’s healing response is less intense for these types of injuries, resulting in a shorter duration of redness and a less noticeable scar.
Skin Type and Genetics
Your skin type and genetic makeup play a crucial role in scar healing. Some people naturally produce more collagen, leading to thicker, more prominent scars. Conversely, others may experience less visible scarring. Understanding your skin type can help set realistic expectations for scar healing.
Individuals with darker skin tones are more prone to developing keloid and hypertrophic scars, which tend to be raised and redder for a longer period. Genetic predispositions can also influence how the body responds to injury and the subsequent healing process.
Moreover, certain genetic factors may affect the skin’s elasticity and ability to regenerate, impacting the overall appearance and duration of a scar’s redness. Being aware of these factors can guide you in choosing appropriate scar management strategies.
Age and Health
Age and overall health also affect scar healing. Younger individuals tend to heal faster, while older adults may experience slower healing due to reduced collagen production and skin elasticity. Additionally, factors like nutrition, hydration, and overall wellness contribute to the body’s ability to heal effectively.
The presence of chronic conditions such as diabetes or autoimmune disorders can further slow the healing process, leading to prolonged redness and scarring. These conditions may impair blood circulation and immune response, both of which are critical for effective wound healing.
Proper wound care, coupled with a healthy lifestyle, can significantly influence the healing timeline. Maintaining a balanced diet rich in vitamins and minerals, staying hydrated, and avoiding smoking can all support the body’s natural healing mechanisms.
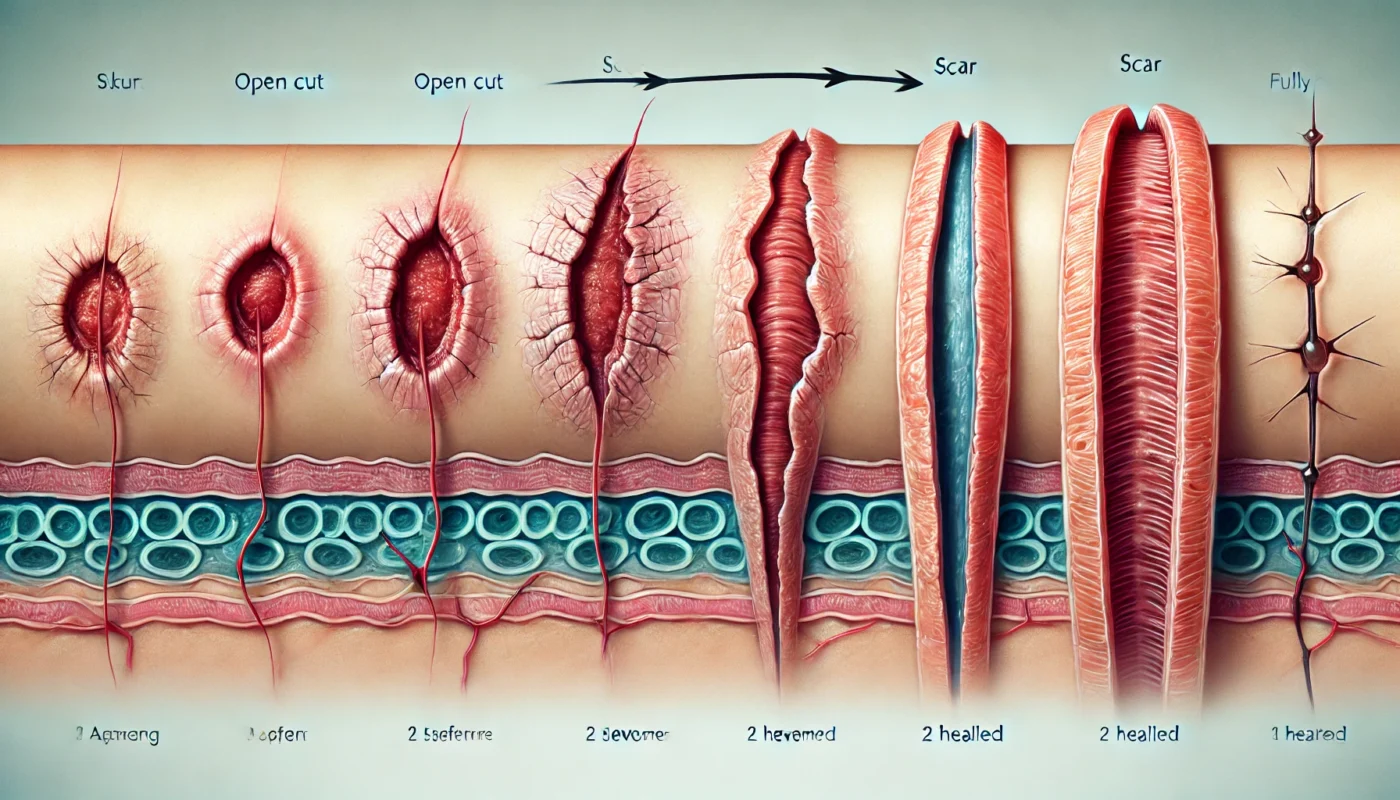
The Scar Healing Timeline
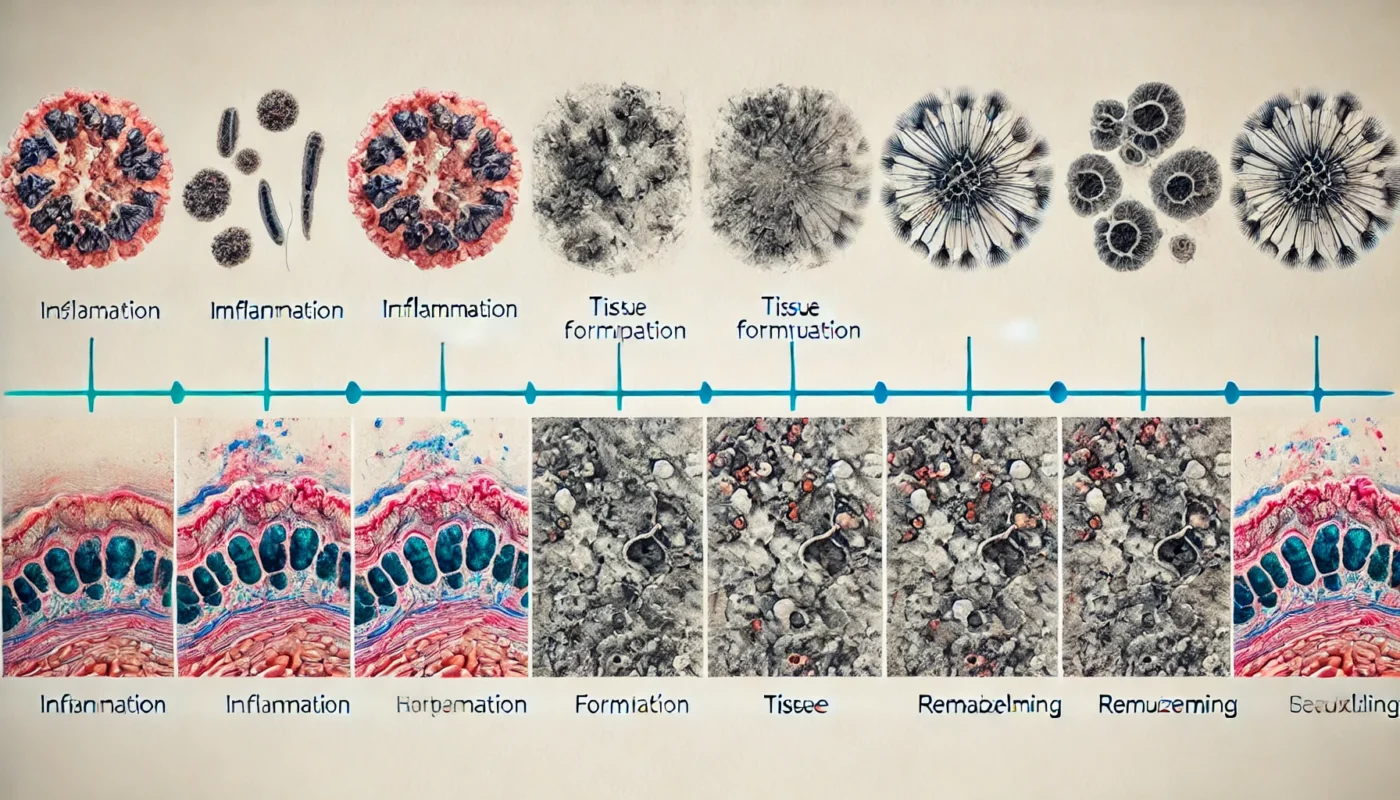
The scar healing timeline can be broken down into several stages, each characterized by distinct physiological processes.
Inflammatory Phase
This initial phase lasts a few days to a week. It’s characterized by redness, swelling, and tenderness as the body sends white blood cells to the injury site to fight infection and begin tissue repair. During this phase, the body’s immune response is activated, and clotting mechanisms work to stop bleeding and protect the wound from further damage.
The influx of blood and immune cells to the site of injury also facilitates the removal of debris and bacteria, preparing the wound for the next stage of healing. This phase is crucial for preventing infection and setting the stage for subsequent tissue regeneration.
Proliferative Phase
Lasting several weeks, this phase involves the production of new tissue and collagen. The wound contracts, and the initial scar forms, often appearing red and raised. During this time, fibroblasts play a key role in synthesizing collagen and extracellular matrix components, which provide structure and support to the newly formed tissue.
Angiogenesis, or the formation of new blood vessels, also occurs during this phase, ensuring an adequate supply of oxygen and nutrients to the healing tissue. As the new tissue matures, the wound edges draw closer together, further reducing the wound size and improving its appearance.
Maturation Phase
This final phase can last several months to a few years. During this time, the scar flattens, fades in color, and becomes less noticeable as collagen reorganizes. The remodelling of collagen fibers enhances the tensile strength of the scar tissue, making it more resilient to mechanical stress.
As the scar matures, the blood vessels recede, contributing to the fading of redness. The scar’s appearance continues to improve as the surrounding skin regains its normal pigmentation and texture. While complete resolution may not be possible, this phase marks a significant improvement in the overall appearance of the scar.
Types of Scars and Their Characteristics
Different types of scars can develop based on the nature of the injury and individual healing responses. Understanding these variations can help in managing expectations and selecting appropriate treatment options.
Hypertrophic Scars
Hypertrophic scars are raised and red, but they do not extend beyond the original wound boundaries. They may improve over time with proper care and treatment. These scars are often the result of excessive collagen production during the healing process, leading to a raised and firm appearance.
While hypertrophic scars can be bothersome, they tend to flatten and fade over time, especially with interventions such as silicone gel sheets, pressure therapy, or steroid injections. Consistent monitoring and appropriate treatment can help accelerate their improvement.
Keloid Scars
Keloids are raised, thick scars that extend beyond the original wound site. They are more common in individuals with darker skin tones and may require medical intervention to improve their appearance. Unlike hypertrophic scars, keloids continue to grow even after the wound has healed, often resulting in a larger and more prominent scar.
Treatment options for keloids include corticosteroid injections, cryotherapy, laser therapy, and surgical excision. However, keloids have a high recurrence rate, necessitating ongoing management and follow-up care.
Atrophic Scars
Atrophic scars are sunken and result from collagen loss during healing. Common examples include acne scars and chickenpox scars. These scars appear as depressions or pits in the skin due to insufficient collagen production during the healing process.
Several treatment modalities, such as dermal fillers, microneedling, and laser resurfacing, can help improve the appearance of atrophic scars by stimulating collagen production and promoting skin rejuvenation. A tailored treatment plan can yield optimal results based on the specific characteristics of the scar.
Contracture Scars
Contracture scars occur when the skin tightens during healing, often affecting mobility. They are typical after burns and may require surgical intervention. These scars form when the skin loses elasticity and contracts, potentially restricting movement and causing functional impairment.
In severe cases, surgical procedures such as skin grafting or tissue expansion may be necessary to release the contracture and restore mobility. Physical therapy and rehabilitation can also play a crucial role in improving function and preventing further complications.

Strategies to Minimize Old Scars
While scars may never completely disappear, several strategies can help minimize their appearance and promote healing.
Topical Treatments
Over-the-counter creams and gels containing silicone, vitamin E, or onion extract can help improve scar texture and color. Consistent application is key to seeing results. Silicone-based products are particularly effective at hydrating the scar tissue and reducing redness and thickness.
In addition to commercially available treatments, natural remedies such as aloe vera and honey may offer soothing and moisturizing benefits, supporting the skin’s healing process. It’s important to consult with a dermatologist to determine the most suitable topical treatment based on your specific needs.
Sun Protection
Protecting scars from sun exposure can prevent them from becoming darker and more noticeable. Use broad-spectrum sunscreen with at least SPF 30 when spending time outdoors. Ultraviolet (UV) rays can exacerbate pigmentation changes in scar tissue, making them more pronounced.
In addition to sunscreen, wearing protective clothing and seeking shade during peak sun hours can help safeguard your skin and minimize the risk of hyperpigmentation. Consistent sun protection is crucial for maintaining the best possible appearance of your scars.
Massage Therapy
Gently massaging the scar tissue can improve blood circulation and help break down excess collagen, reducing scar height and rigidity. Regular massage can also enhance the skin’s flexibility and promote a smoother texture.
Massage therapy can be particularly beneficial for hypertrophic and contracture scars, as it encourages the remodeling of collagen fibers and helps prevent the formation of adhesions. Consulting with a physical therapist or massage therapist can provide guidance on effective techniques.
Professional Treatments
For more severe scars, professional treatments like laser therapy, microdermabrasion, or corticosteroid injections may be recommended by a dermatologist or plastic surgeon. These interventions can significantly improve the appearance of scars by targeting specific skin layers and promoting collagen remodeling.
Laser therapy, for example, can reduce redness and improve texture by stimulating new collagen production, while microdermabrasion can exfoliate the skin’s surface and enhance its smoothness. A personalized treatment plan can yield optimal results based on the severity and type of scar.

Can Scars Go Away Completely?
While it’s unlikely for scars to disappear entirely, they often fade over time and become less noticeable. The extent to which a scar fades depends on various factors, including its type, location, and the individual’s skin characteristics. Patience and consistent care are essential for optimal results.
The natural aging process, combined with proper skincare and professional interventions, can lead to significant improvements in the appearance of scars. While complete eradication may not be possible, the goal is to achieve a scar that is less visible and more harmonious with the surrounding skin.
It’s important to set realistic expectations and understand that scar healing is a gradual process. With time and effort, many individuals find that their scars become a less prominent aspect of their skin’s landscape.
Conclusion
Scars are a natural part of the body’s healing process, and their duration and appearance can vary widely based on multiple factors. By understanding the scar healing timeline and implementing effective strategies, you can take proactive steps to improve healing outcomes and minimize the visibility of scars.
Whether you’re dealing with a minor cut or a surgical incision, staying informed and practicing good skincare can make a significant difference in the healing journey. Remember, every scar tells a story, and with the right care, they can become a less prominent chapter in your life. Consistent effort and a positive attitude towards your skin’s recovery can empower you to embrace your scars as a testament to your resilience and healing journey.
Further Reading:
Scarring After Plastic Surgery: Everything You Need to Know
Scar Management after Burn Injury
Contracture scars, scar treatment, skin healing, topical treatments, sun protection, massage therapy, professional treatments, laser therapy, microdermabrasion, scar management, dermatology, physical therapy, skincare, scar appearance, healing process
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.