Patellar tendonitis, often referred to as “jumper’s knee,” is a common overuse injury affecting the patellar tendon, which connects the kneecap (patella) to the shinbone (tibia). This condition is prevalent among athletes who engage in repetitive jumping or running activities, but it can also affect non-athletes. Left untreated, patellar tendonitis can progress, leading to chronic pain and limitations in mobility. This article delves into the symptoms, causes, treatment options, prevention strategies, and the role of nutritional supplements in managing and recovering from patellar tendonitis.
You May Also Like:
What Is Patellar Tendonitis?
Patellar tendonitis is characterized by inflammation and degeneration of the patellar tendon, which plays a crucial role in knee extension. This tendon endures significant stress during activities such as jumping, running, and squatting. The injury often begins as mild discomfort but can progress into a more severe condition known as patellar tendinopathy if not managed properly.

Symptoms of Patellar Tendonitis
The symptoms of patellar tendonitis can vary depending on the severity of the condition. Common signs include:
- Anterior Knee Pain: Pain is typically localized below the kneecap and intensifies during physical activities like jumping or climbing stairs.
- Stiffness: Morning stiffness or difficulty moving the knee after prolonged inactivity.
- Swelling: Mild swelling around the patellar tendon.
- Tenderness: Pain when pressing on the affected tendon.
- Reduced Functionality: Difficulty performing athletic activities or daily tasks due to pain and weakness.
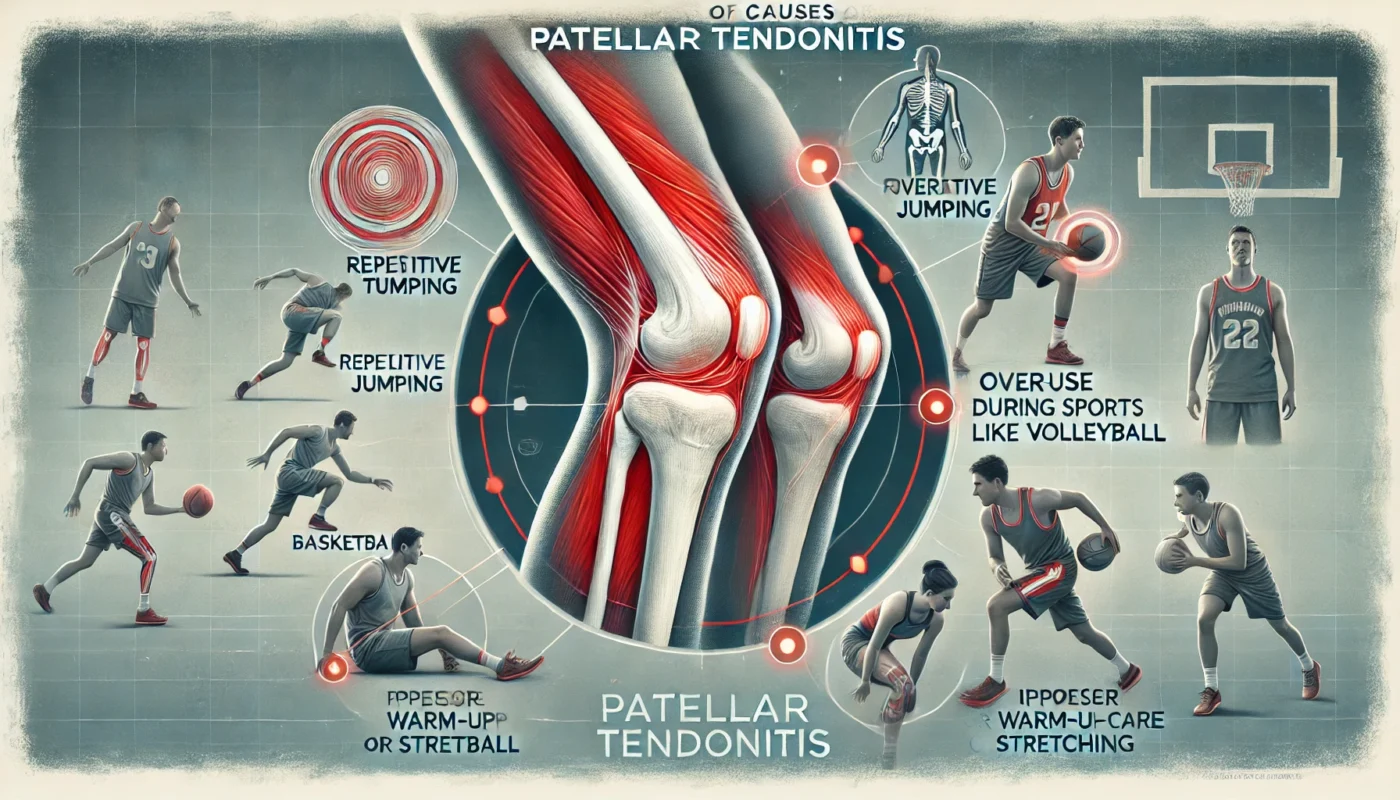
Causes of Patellar Tendonitis
Patellar tendonitis is primarily caused by repetitive strain and microtrauma to the patellar tendon. Contributing factors include:
1. Overuse
Repetitive jumping or running can lead to microtears in the tendon. A study published in Sports Medicine (2019) found that athletes involved in sports like basketball and volleyball have a higher prevalence of patellar tendonitis due to repetitive high-impact movements.
2. Muscle Imbalances
Weak or tight quadriceps and hamstrings can place excessive stress on the patellar tendon. Research in The Journal of Sports Science and Medicine (2018) emphasized that athletes with muscle imbalances are more prone to developing overuse injuries, including patellar tendonitis.
3. Poor Technique
Improper landing techniques during jumping or running can increase strain on the tendon. A study in Biomechanics (2020) highlighted that faulty movement patterns significantly contribute to the development of patellar tendonitis.
4. Inadequate Recovery
Insufficient rest or recovery periods between high-intensity activities can prevent proper tendon repair, increasing the risk of injury.
5. Structural Abnormalities
Flat feet, high arches, or misalignment of the knee joint can predispose individuals to patellar tendonitis.
Treatment Options for Patellar Tendonitis Recovery
The treatment of patellar tendonitis focuses on reducing pain and inflammation, promoting tendon healing, and preventing recurrence. Options range from conservative measures to advanced therapies:
1. Rest and Activity Modification
Avoiding high-impact activities allows the patellar tendon to heal. Substituting low-impact exercises like swimming or cycling can help maintain fitness while minimizing strain.
2. Pain Management
- Ice Therapy: Applying ice packs for 15–20 minutes several times a day reduces inflammation and alleviates pain.
- NSAIDs: Nonsteroidal anti-inflammatory drugs may be prescribed to manage pain and swelling.
3. Physical Therapy
A structured rehabilitation program is critical for recovery. Exercises focus on:
- Eccentric Strengthening: Controlled lowering movements of the quadriceps to strengthen the patellar tendon. A study in The American Journal of Sports Medicine (2018) found that eccentric exercises significantly reduced pain and improved functionality in individuals with patellar tendonitis.
- Flexibility Training: Stretching the quadriceps and hamstrings to alleviate tension on the tendon.
- Manual Therapy: Techniques such as massage or myofascial release to improve circulation and mobility.
4. Shockwave Therapy
Extracorporeal shockwave therapy (ESWT) uses sound waves to stimulate tendon healing. A clinical trial in Orthopaedic Journal of Sports Medicine (2021) demonstrated that ESWT improved pain and function in patients with chronic patellar tendonitis.
5. Platelet-Rich Plasma (PRP) Injections
PRP injections involve using a patient’s own platelets to promote tissue healing. Research in The Journal of Orthopaedic Research (2019) reported positive outcomes in terms of pain relief and tendon repair with PRP therapy.
6. Surgical Intervention
For severe or chronic cases unresponsive to conservative treatment, surgery may be necessary to remove damaged tissue and promote healing.
7. Nutritional Support
Proper nutrition and supplementation can accelerate recovery and enhance tendon health, as discussed below.
Nutritional Supplementation for Patellar Tendonitis Relief
Certain supplements can support tendon healing, reduce inflammation, and improve overall recovery. The following are particularly effective for patellar tendonitis:
1. Collagen Peptides
Collagen provides the building blocks necessary for tendon repair. A study in Sports Medicine (2020) found that collagen supplementation improved tendon strength and reduced recovery time in athletes with overuse injuries.
2. Bromelain
Bromelain, an enzyme derived from pineapple, has anti-inflammatory properties. A clinical trial published in Clinical Rheumatology (2017) demonstrated that bromelain supplementation reduced swelling and improved recovery in individuals with soft tissue injuries.
3. Magnesium Glycinate
Magnesium is essential for muscle relaxation and tissue repair. A randomized controlled trial published in Magnesium Research (2014) reported that magnesium supplementation reduced muscle tension and supported recovery from tendon-related injuries.
4. Vitamin C
Vitamin C plays a key role in collagen synthesis and tissue healing. Research in The American Journal of Clinical Nutrition (2018) found that adequate vitamin C intake enhanced recovery in individuals with tendon injuries.
5. Omega-3 Fatty Acids
Omega-3s are known for their anti-inflammatory effects. A study in The Journal of Sports Science and Medicine (2016) showed that omega-3 supplementation decreased recovery times and reduced pain in athletes with tendonitis.

Healing Strategies for Patellar Tendonitis
Incorporating additional strategies into the recovery plan can optimize healing and prevent recurrence:
1. Gradual Strength Training
Introducing controlled resistance exercises helps rebuild tendon strength and resilience while avoiding re-injury.
2. Proper Warm-Up
Engaging in dynamic stretches and warm-up exercises prepares the tendon for physical activity.
3. Foam Rolling
Using a foam roller on the quadriceps and surrounding muscles can alleviate tension and improve circulation.
4. Adequate Sleep
Rest is critical for tissue repair and overall recovery.
5. Hydration
Staying hydrated promotes optimal tendon function and reduces stiffness.
Steps for Possible Prevention of Patellar Tendonitis
Preventing patellar tendonitis involves proactive measures to reduce strain on the tendon and maintain overall knee health:
1. Strengthen the Quadriceps and Hamstrings
Incorporating exercises that target the thigh muscles improves knee stability and reduces stress on the patellar tendon.
2. Use Proper Techniques
Practicing correct landing and jumping techniques minimizes the risk of overuse injuries.
3. Wear Supportive Footwear
Shoes with proper cushioning and arch support reduce impact forces on the knees.
4. Gradually Increase Activity Levels
Avoid sudden increases in training intensity or volume to prevent overloading the tendon.
5. Include Regular Stretching
Stretching the quadriceps, hamstrings, and calf muscles improves flexibility and reduces tension on the patellar tendon.
Conclusion
Patellar tendonitis is a common overuse injury that can cause significant pain and limit physical activity if left untreated. Recovery requires a comprehensive approach, including rest, physical therapy, and in severe cases, advanced therapies such as PRP injections or surgery. Nutritional supplements like collagen peptides, bromelain, and magnesium glycinate play a vital role in reducing inflammation and promoting tendon repair. By adopting proper prevention strategies, including strength training, technique refinement, and gradual activity progression, individuals can minimize the risk of patellar tendonitis and maintain optimal knee health. With the right combination of treatments and preventive measures, recovery is achievable, and recurrence can be prevented.

References
- Efficacy of Vitamin C Supplementation on Collagen Synthesis and Oxidative Stress After Musculoskeletal Injuries: A Systematic Review. Retrieved from: https://pubmed.ncbi.nlm.nih.gov/30386805/
- Bromelain as a Treatment for Osteoarthritis: a Review of Clinical Studies. Retrieved from: https://pmc.ncbi.nlm.nih.gov/articles/PMC538506/
- Effects of magnesium supplementation on muscle soreness in different type of physical activities: a systematic review. Retrieved from: https://pubmed.ncbi.nlm.nih.gov/38970118/
- Effect of high-dose vitamin C and E supplementation on muscle recovery and training adaptation: a mini review. Retrieved from: https://pmc.ncbi.nlm.nih.gov/articles/PMC10440181/
- Effects of Omega-3 Fatty Acids on Muscle Mass, Muscle Strength and Muscle Performance among the Elderly: A Meta-Analysis. Retrieved from: https://pmc.ncbi.nlm.nih.gov/articles/PMC7761957/
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.

