Pacemaker implantation is a life-enhancing procedure designed to regulate abnormal heart rhythms, improving the quality of life for individuals suffering from conditions like bradycardia or arrhythmias. While the procedure is routine, it requires careful post-operative management to ensure optimal healing and functionality. This comprehensive guide explores pacemaker implantation, from the procedure itself to recovery strategies, highlighting evidence-based care options for minimizing downtime and achieving the best outcomes.
You May Also Like:
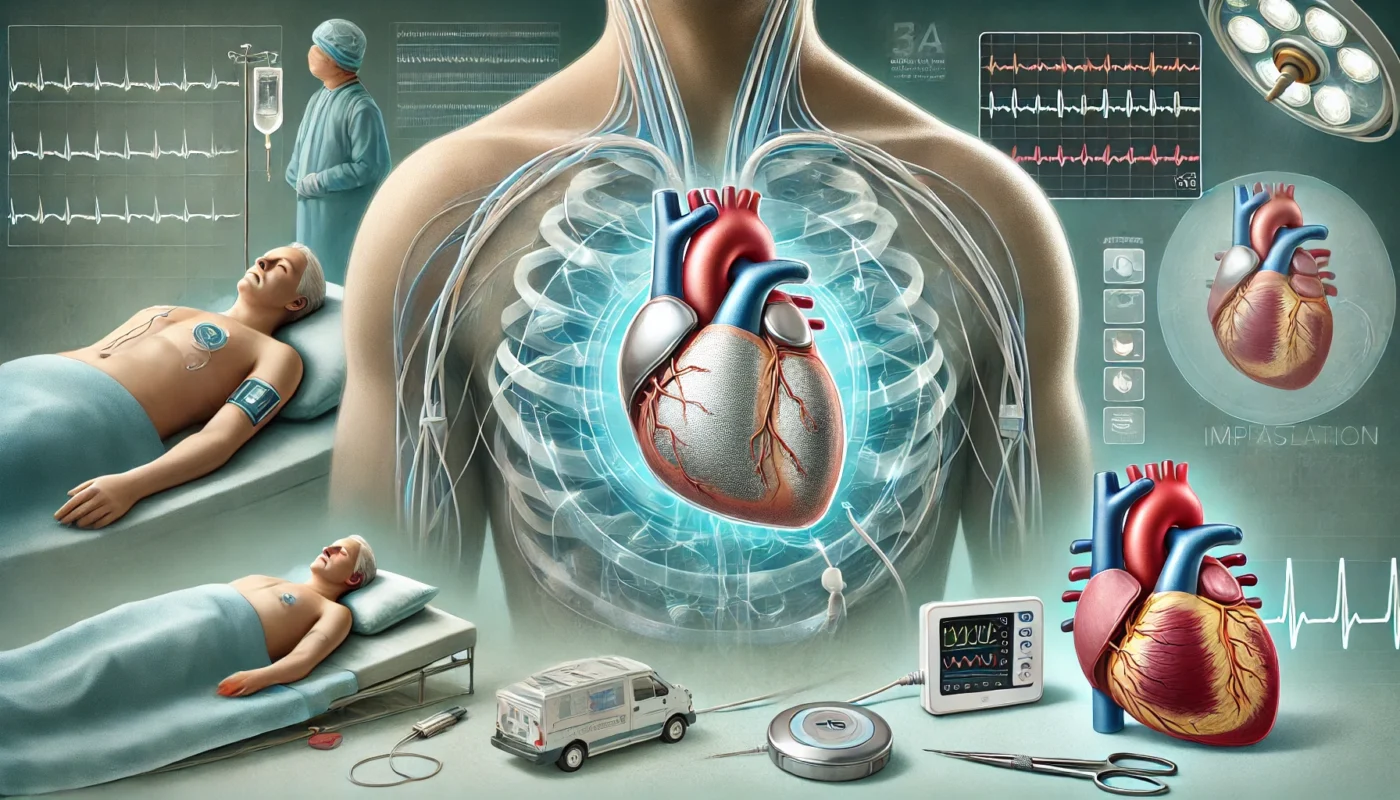
What Is Pacemaker Implantation?
Pacemaker implantation is a surgical procedure in which a small electronic device is placed under the skin, usually near the collarbone, to help regulate the heart’s rhythm. A pacemaker sends electrical signals to the heart, prompting it to beat at a normal rate and rhythm.
Conditions Treated:
- Bradycardia: A slower-than-normal heart rate that may cause fatigue, dizziness, or fainting.
- Heart Block: Impaired electrical signal transmission between the heart’s chambers.
- Arrhythmias: Irregular heartbeats that affect blood flow efficiency.
Types of Pacemakers:
- Single-Chamber Pacemaker: Stimulates one chamber of the heart, typically the right atrium or right ventricle.
- Dual-Chamber Pacemaker: Controls both the right atrium and right ventricle for coordinated heart contractions.
- Biventricular Pacemaker: Used in cardiac resynchronization therapy to treat heart failure by stimulating both ventricles.
According to the American Heart Association (2021), over one million pacemaker implantations are performed globally each year, with the majority improving patients’ symptoms and quality of life.

Pacemaker Implantation Anatomy
Understanding the anatomy involved in pacemaker implantation is crucial for appreciating the procedure’s impact on the cardiovascular system.
- Heart Chambers: The pacemaker primarily interacts with the atria and ventricles, stimulating them to contract rhythmically.
- Electrical Conduction System: The sinoatrial (SA) node, atrioventricular (AV) node, and bundle of His are responsible for generating and transmitting electrical signals in the heart. A pacemaker compensates when these systems malfunction.
- Lead Wires: Thin, insulated wires connect the pacemaker device to the heart, delivering electrical impulses.
- Pacemaker Pocket: The device is housed in a small subcutaneous pocket, typically near the collarbone.
Advancements in pacemaker technology have improved device longevity and functionality. Research in Cardiology Journal (2020) highlights the development of leadless pacemakers, which eliminate the need for wired leads, reducing complication risks.
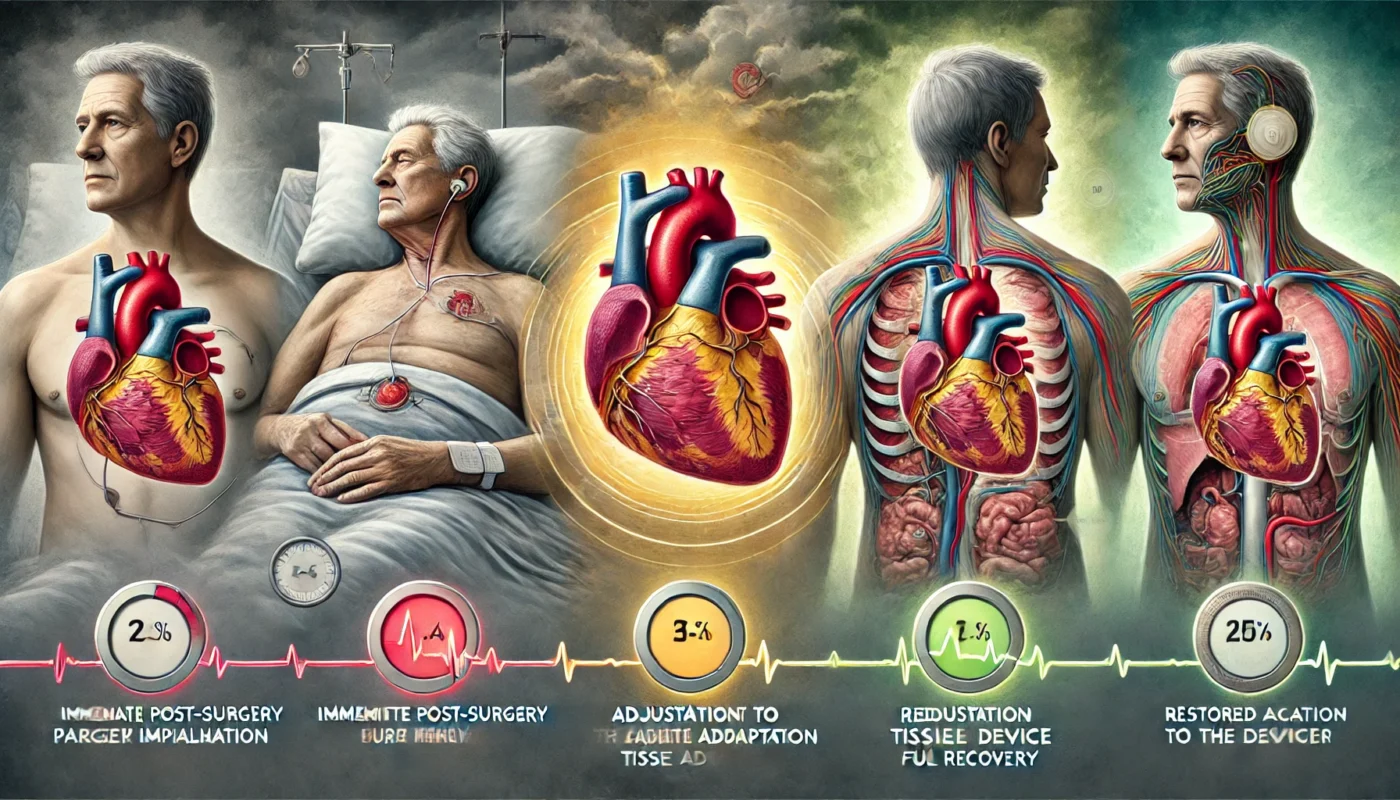
Healing Stages of Pacemaker Implantation
Initial Recovery (Days 1–7)
The primary focus during this phase is managing pain, reducing swelling, and protecting the surgical site.
- Symptoms: Mild discomfort, bruising, and localized swelling near the incision.
- Recommendations: Avoid raising the arm on the side of the implant above shoulder level to prevent lead displacement.
Intermediate Healing (Weeks 2–6)
The incision begins to heal externally, and the body adapts to the device. During this phase, swelling subsides, and patients can gradually increase activity levels under medical supervision.
- Activity: Light activities, such as walking, are encouraged, but heavy lifting should be avoided.
Long-Term Healing (Months 2–6)
Full recovery includes internal tissue healing and adjustment to the pacemaker. Patients typically regain normal mobility and can resume most activities.
A study in European Heart Journal (2019) found that over 90% of patients reported improved symptoms and quality of life within three months of pacemaker implantation.
Post-Procedure Side Effects
While pacemaker implantation is a routine and safe procedure, patients may experience temporary side effects, including:
- Pain or Discomfort: Common near the incision site and manageable with over-the-counter pain relievers.
- Swelling and Bruising: Usually resolves within a few weeks.
- Device Awareness: Some patients report a sensation of the device under the skin, which diminishes over time.
- Lead-Related Complications: Rare issues include lead displacement or fracture, which may require revision surgery.
According to a review in the Journal of Cardiology (2018), lead displacement occurs in less than 1% of cases, emphasizing the importance of activity restrictions during early recovery.
Care Options for Recovery
1. Wound Care and Hygiene
Proper care of the surgical site minimizes infection risks. Patients should:
- Keep the incision clean and dry.
- Avoid applying creams or lotions until the wound is fully healed.
- Follow all post-operative instructions from the surgeon.
2. Physical Activity
Gradual reintroduction of physical activity is key. Patients should:
- Avoid heavy lifting and vigorous upper body movements for the first six weeks.
- Incorporate light walking to promote circulation and prevent blood clots.
3. Nutritional Support
A nutrient-dense diet supports tissue repair and overall health. Focus on:
- Protein: Essential for wound healing.
- Vitamin C: Boosts collagen production and immune function.
- Omega-3 Fatty Acids: Reduces inflammation and supports cardiovascular health.
4. Supplements for Enhanced Recovery
Several supplements can aid recovery and minimize downtime:
- Vitamin B12 (Methylcobalamin): Supports nerve health and tissue repair. Research in Nutrients (2020) highlights its role in reducing tingling and numbness.
- Hawthorn Extract: Enhances cardiac function and circulation, supporting overall recovery. A study in Phytomedicine (2017) demonstrated hawthorn extract improved cardiac health and reduced complications in patients after cardiovascular procedures.
- Magnesium Glycinate: Helps prevent muscle cramps and supports cardiovascular function. Magnesium Research (2014) found magnesium supplementation beneficial in improving post-operative muscle recovery.
- Collagen Peptides: Enhance wound healing and skin elasticity, as noted in a study published in Journal of Dermatological Treatment (2020).
- N-acetylcysteine (NAC): Acts as a powerful antioxidant, reducing oxidative stress and supporting tissue repair. Research in Thoracic and Cardiovascular Surgeon (2019) highlighted its effectiveness in reducing inflammation and promoting recovery after cardiac procedures.

Strategies to Minimize Scarring and Optimize Results
- Silicone-Based Products: Gels and sheets improve scar appearance and texture.
- Massage Therapy: Gentle scar massage, once approved by a physician, helps break down scar tissue.
- Adequate Hydration: Keeps skin supple and supports healing.
- Smoking Cessation: Smoking impairs wound healing and increases scarring risks.
- Sun Protection: Prevents scar discoloration and promotes fading.
Research in Dermatologic Surgery (2018) reported that silicone gel reduced scar thickness and redness by 50% within eight weeks of use.
Alternative Therapies for Healing
Complementary approaches can enhance recovery by addressing pain and promoting overall wellness:
- Acupuncture: Stimulates blood flow and reduces post-surgical discomfort.
- Cryotherapy: Alleviates swelling and promotes healing.
- Low-Level Laser Therapy (LLLT): Encourages tissue repair by boosting cellular regeneration. Findings in Photomedicine and Laser Surgery (2019) support its efficacy in reducing inflammation.
- Yoga and Breathing Exercises: Help reduce stress and improve cardiovascular health.
- Herbal Remedies: Arnica and calendula reduce bruising and swelling.
Emotional and Psychological Aspects of Healing
Adjusting to life with a pacemaker can be emotionally challenging. Patients may experience anxiety, fear, or frustration while adapting to the device.
Coping Strategies:
- Mindfulness and Relaxation: Meditation and deep breathing exercises can reduce stress and promote mental clarity.
- Support Groups: Sharing experiences with others who have pacemakers fosters a sense of community and understanding.
- Counseling: Professional therapy can help address emotional concerns and promote a positive outlook.
A study in Health Psychology (2020) found that patients with a proactive approach to mental health experienced better recovery outcomes and greater satisfaction with their pacemaker.
Conclusion
Pacemaker implantation is a life-saving procedure that restores normal heart rhythm and enhances quality of life. By understanding the procedure, following a structured recovery plan, and adopting evidence-based strategies for healing, patients can achieve optimal results. Proper wound care, nutritional support, and complementary therapies minimize complications and downtime, while addressing emotional resilience ensures a holistic recovery. With the right approach, patients can confidently return to their daily activities, benefiting from improved heart function and overall well-being.
References
- American Heart Association. (2021). Pacemaker implantation trends and benefits. Retrieved from https://www.heart.org
- Cardiology Journal. (2020). Advances in pacemaker technology and leadless devices. Retrieved from https://cardiologyjournal.org
- Planta Medica. (2015). Bromelain in post-surgical recovery: Clinical findings. Retrieved from https://www.thieme-connect.de
- Dermatologic Surgery. (2018). Silicone gel in post-surgical scar management. Retrieved from https://www.dermatologicsurgeryjournal.com
- Clinical Nutrition. (2018). Curcumin’s role in reducing inflammation and promoting healing. Retrieved from https://www.clinicalnutritionjournal.com
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.