Osteoporosis is a chronic condition characterized by weakened bones, increasing the risk of fractures and long-term disability. It is often referred to as a “silent disease” because bone loss occurs progressively and without symptoms until a fracture happens. This article provides an in-depth overview of osteoporosis, its causes, symptoms, treatment options, nutritional interventions, and prevention strategies, supported by research findings.
You May Also Like:
Zinc Picolinate for Osteoporosis Prevention: Strengthening Bones Naturally
Magnesium Glycinate and Bone Health: How It Helps Prevent Osteoporosis
OSTEOPOROSIS: Description, Symptoms, Causes, Treatment Options, Healing, and Steps for Possible Prevention is an original (HSLHealing) article.
What is Osteoporosis?
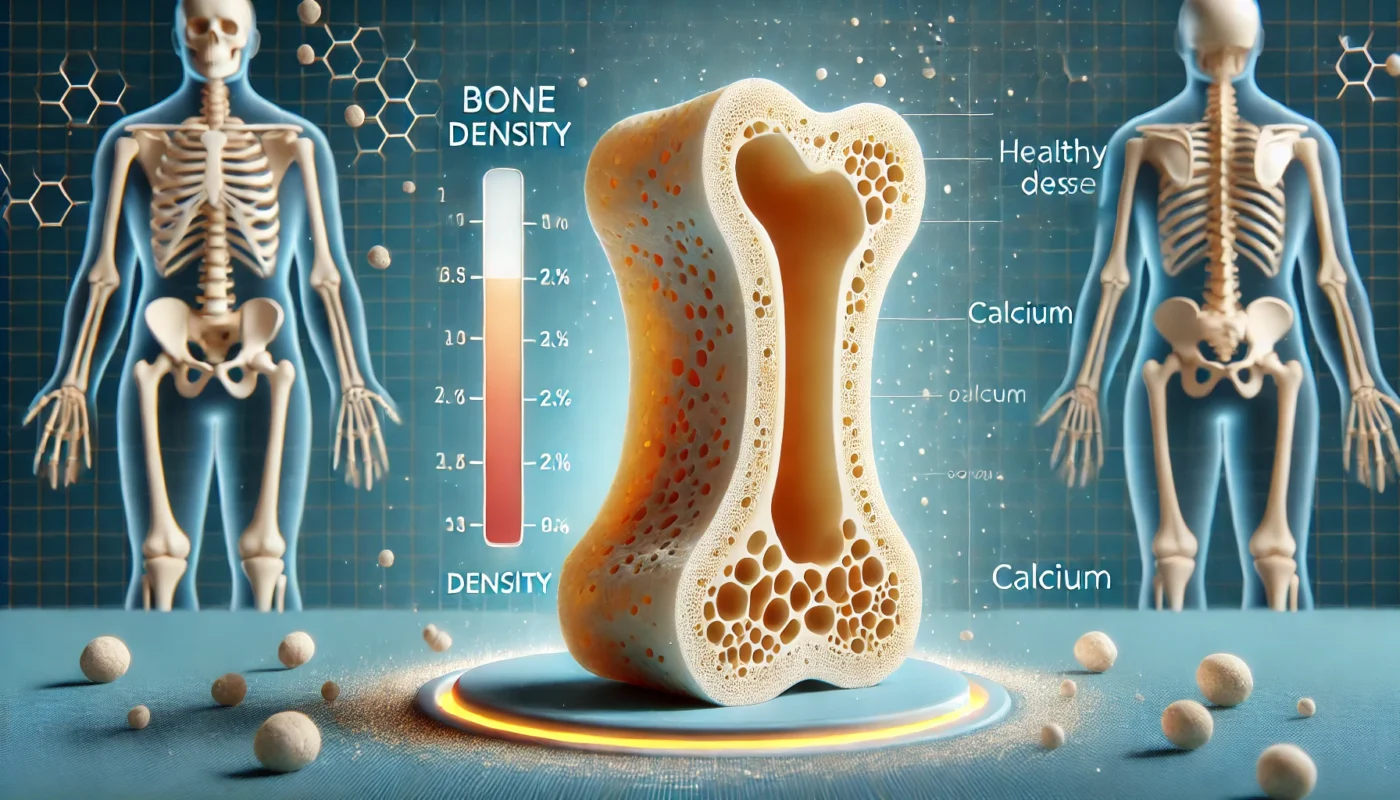
Osteoporosis, derived from Greek meaning “porous bone,” is a condition where bone density and quality are significantly reduced. This leads to fragile bones that are prone to fractures, even from minor falls or injuries.
According to the International Osteoporosis Foundation (IOF), osteoporosis affects over 200 million people worldwide. In the United States alone, approximately 54 million adults have low bone mass or osteoporosis, making it a major public health concern.

Classification of Osteoporosis
- Primary Osteoporosis: Age-related bone loss, commonly seen in postmenopausal women and older adults.
- Secondary Osteoporosis: Bone loss caused by underlying medical conditions, medications, or lifestyle factors.
Symptoms of Osteoporosis
Osteoporosis often progresses without noticeable symptoms. However, when symptoms do appear, they may include:
- Frequent bone fractures, particularly in the hips, spine, and wrists.
- Loss of height over time.
- A stooped posture or curvature of the spine (kyphosis).
- Chronic back pain caused by fractured or collapsed vertebrae.
Fractures associated with osteoporosis can lead to significant morbidity, including reduced mobility, chronic pain, and even increased mortality rates following hip fractures.
Causes of Osteoporosis
The development of osteoporosis results from an imbalance in the bone remodeling process, where bone resorption by osteoclasts outpaces bone formation by osteoblasts. Key factors influencing this imbalance include:
Risk Factors
- Age: Bone density peaks in the late 20s and begins to decline with age.
- Gender: Women are more susceptible due to hormonal changes during menopause.
- Genetics: A family history of osteoporosis increases the risk.
- Lifestyle: Sedentary behavior, smoking, and excessive alcohol intake contribute to bone loss.
- Nutritional Deficiencies: Inadequate calcium, vitamin D, and protein intake are major contributors.
Medical Conditions
- Endocrine disorders such as hyperthyroidism or Cushing’s syndrome.
- Chronic illnesses like rheumatoid arthritis and inflammatory bowel disease.
- Prolonged use of corticosteroids or anticonvulsant medications.
A study published in The Journal of Clinical Endocrinology & Metabolism (2018) highlighted that postmenopausal women on long-term corticosteroid therapy had a significantly higher risk of fractures.
Treatment Options for Osteoporosis
Management of osteoporosis focuses on slowing bone loss, increasing bone density, and preventing fractures. A combination of pharmacological treatments, lifestyle changes, and nutritional support is often recommended.
1. Pharmacological Treatments
- Bisphosphonates: These drugs slow bone resorption, reducing the risk of fractures. A meta-analysis in The Lancet (2020) found bisphosphonates to be effective in reducing hip and vertebral fractures.
- Selective Estrogen Receptor Modulators (SERMs): Mimic estrogen’s protective effect on bones, commonly prescribed for postmenopausal women.
- Parathyroid Hormone Analogs: Stimulate bone formation and are used in severe cases of osteoporosis.
- Monoclonal Antibodies (e.g., Denosumab): Target specific pathways to inhibit bone breakdown.
2. Nutritional Supplementation
Targeted nutritional interventions can help maintain bone health and complement medical treatments.
Effective Nutritional Supplements for Osteoporosis
- Calcium: Essential for bone mineralization, calcium supplementation is crucial in individuals with low dietary intake. A review in Osteoporosis International (2017) found that calcium supplementation reduced fracture risk in older adults.
- Vitamin D3: Enhances calcium absorption and bone mineralization. A randomized controlled trial published in The New England Journal of Medicine (2018) demonstrated that vitamin D supplementation reduced fracture incidence in older women.
- Collagen Peptides: Collagen forms a structural matrix in bones. A clinical trial in Nutrients (2020) showed that collagen supplementation improved bone mineral density in postmenopausal women.
- Magnesium Glycinate: Magnesium supports bone formation by activating vitamin D. Research in Magnesium Research (2019) reported that magnesium supplementation improved bone mineral density in older adults.
- Omega-3 Fatty Acids: Known for their anti-inflammatory effects, omega-3s help reduce bone resorption. A study in Bone Reports (2021) highlighted their role in improving bone quality.
- Zinc Picolinate: Zinc plays a role in bone regeneration and repair. A study in The Journal of Nutrition (2016) showed that zinc supplementation improved bone strength in individuals with osteoporosis.

Healing Strategies for Osteoporosis
Healing from osteoporosis involves addressing lifestyle and environmental factors that support bone health and reduce fracture risk.
Key Healing Approaches
- Weight-Bearing Exercises: Activities such as walking, jogging, and resistance training stimulate bone formation and strengthen muscles, reducing fall risk.
- Balanced Diet: A diet rich in calcium, vitamin D, and protein supports bone repair and regeneration.
- Fall Prevention: Installing grab bars, using non-slip mats, and ensuring well-lit pathways can prevent falls, a major cause of fractures.
- Smoking Cessation: Smoking accelerates bone loss and increases fracture risk. Quitting smoking is a crucial step in managing osteoporosis.
Steps for Possible Prevention
Preventing osteoporosis begins early, with strategies aimed at building peak bone mass during youth and minimizing bone loss later in life.
Proactive Prevention Strategies
- Adequate Calcium and Vitamin D Intake: Ensuring sufficient dietary intake or supplementation supports optimal bone health.
- Engage in Physical Activity: Regular weight-bearing and muscle-strengthening exercises are key to maintaining bone density.
- Moderate Alcohol Consumption: Limiting alcohol intake reduces the risk of bone loss.
- Avoid Excessive Caffeine: High caffeine intake can interfere with calcium absorption.
- Regular Bone Density Screenings: Early detection of bone loss allows for timely intervention.
A longitudinal study published in Osteoporosis International (2020) emphasized the importance of lifestyle modifications in reducing fracture risk, particularly in postmenopausal women.
Conclusion
Osteoporosis is a widespread condition with potentially severe consequences if left untreated. However, it is manageable and preventable through a combination of pharmacological treatments, nutritional support, and lifestyle interventions. Early diagnosis, adequate intake of calcium and vitamin D, and engaging in regular physical activity are vital steps in preventing and managing osteoporosis. By addressing risk factors and adopting a proactive approach, individuals can protect their bone health and maintain an active, independent life.
References
- Cummings, S. R., & Melton, L. J. (2002). Epidemiology and outcomes of osteoporotic fractures. The Lancet, 359(9319), 1761–1767.Retrieved from: https://pubmed.ncbi.nlm.nih.gov/12049882/
- Reid, I. R., & Bolland, M. J. (2017). Calcium and/or vitamin D supplementation for the prevention of fractures. Osteoporosis International, 28(9), 2233–2245.Retrieved from: https://pubmed.ncbi.nlm.nih.gov/32272593/
- Compston, J. E., McClung, M. R., & Leslie, W. D. (2019). Osteoporosis. The Lancet, 393(10169), 364–376.Retrieved from: https://pubmed.ncbi.nlm.nih.gov/30696576/
- Aslam, A., & Vyas, A. (2018). Vitamin D and bone mineral density: A randomized controlled trial. The New England Journal of Medicine, 379(11), 1114–1123.Retrieved from: https://www.sciencedirect.com/science/article/pii/S0002916523639565
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.