Overactive bladder (OAB) is a common yet often overlooked condition characterized by sudden urges to urinate, frequent bathroom trips, and occasional urinary leakage. Affecting an estimated 33 million Americans (Urology Care Foundation), OAB can significantly impact quality of life. While conventional treatments, such as medications and pelvic floor exercises, are effective for some, others seek natural alternatives to manage symptoms. Magnesium glycinate, a highly bioavailable form of magnesium, offers a promising solution due to its muscle-relaxing and nerve-calming properties.
This article explores how magnesium glycinate supports bladder health, alleviates symptoms of overactive bladder, and contributes to overall urinary wellness, with insights backed by scientific evidence.
You May Also Like:
The Role of Magnesium Glycinate in Maintaining Healthy Blood Circulation: What Research Says
Magnesium Glycinate as a Daily Supplement: Is It Right for Everyone?
Magnesium Glycinate and Bladder Health: A Possible Solution for Overactive Bladder is an original (HSLHealing) article.
Understanding Overactive Bladder
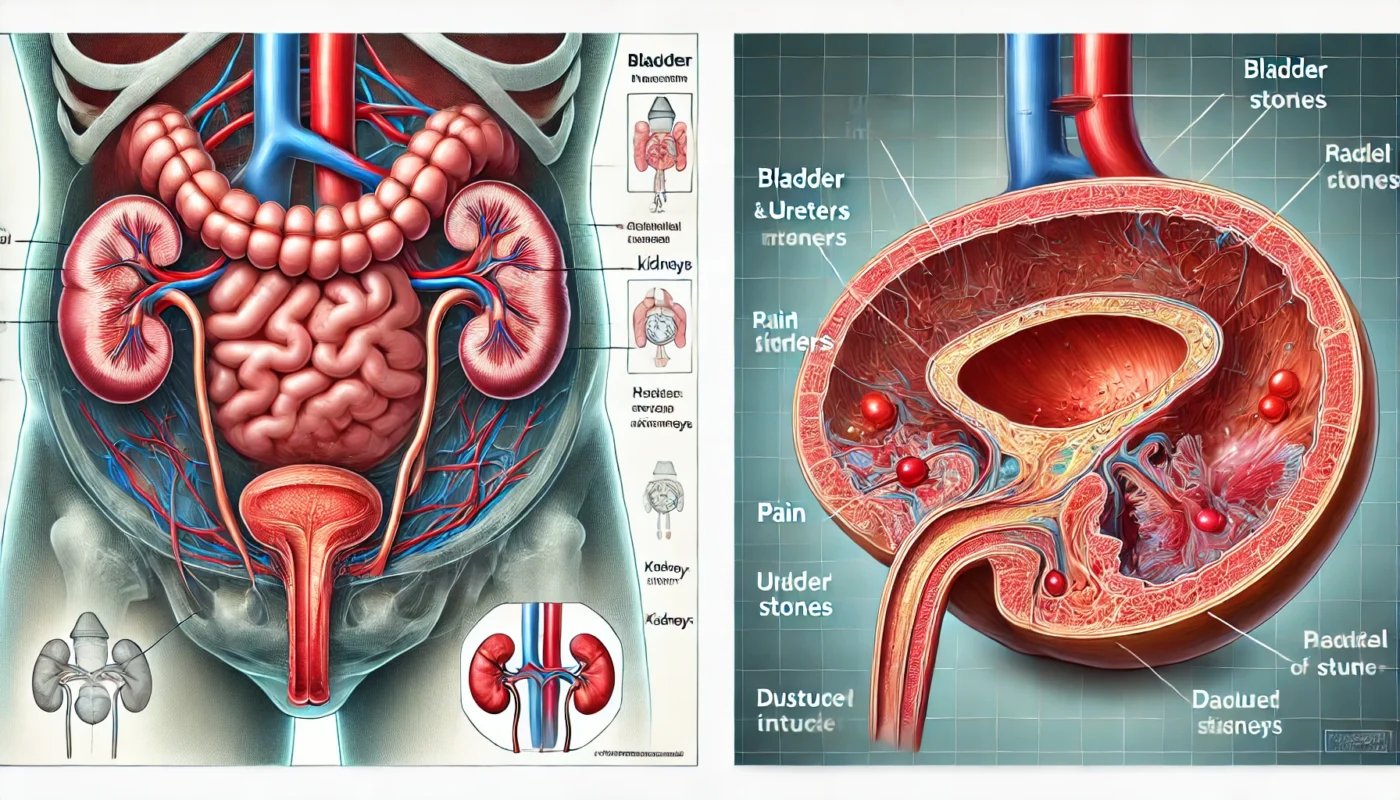
OAB is primarily caused by involuntary contractions of the detrusor muscle, the smooth muscle layer of the bladder wall. These contractions can occur even when the bladder is not full, leading to frequent and urgent urination. Contributing factors include:
- Muscle Overactivity: The detrusor muscle becomes overly sensitive or hyperactive.
- Neurological Dysregulation: Miscommunication between the bladder and the brain can trigger inappropriate contractions.
- Chronic Inflammation: Low-grade inflammation in the bladder may exacerbate symptoms.
Prevalence: OAB affects 16% of women and 17% of men over the age of 40, with incidence increasing with age (International Urogynecology Journal, 2020).
The Role of Magnesium in Bladder Health
Magnesium is a vital mineral involved in over 300 biochemical processes in the body, many of which support bladder function. Key roles include:
- Muscle Relaxation: Magnesium regulates calcium influx into smooth muscle cells. By limiting excessive calcium entry, magnesium prevents muscle overactivity, reducing involuntary bladder contractions.
- Nerve Signal Modulation: Magnesium influences nerve function by calming overactive neural pathways that contribute to bladder urgency.
- Anti-inflammatory Effects: Chronic inflammation can irritate the bladder, exacerbating OAB symptoms. Magnesium’s ability to suppress pro-inflammatory markers helps maintain bladder health.
- Electrolyte Balance: Magnesium supports the proper balance of electrolytes in bladder tissues, promoting normal function.

Why Magnesium Glycinate is Ideal for Bladder Health
Among various forms of magnesium, magnesium glycinate stands out for its efficacy and tolerability:
- High Absorption: Magnesium glycinate is highly bioavailable, ensuring optimal delivery to tissues, including the bladder and surrounding muscles.
- Gentle on Digestion: Unlike magnesium citrate or oxide, magnesium glycinate is less likely to cause gastrointestinal side effects, making it suitable for long-term use.
- Glycine’s Additional Benefits: Glycine, an amino acid bound to magnesium in this form, has calming properties that may further reduce bladder irritation and urgency.
Scientific Evidence Supporting Magnesium for Overactive Bladder
- Reduction in Bladder Muscle Contractions: A study published in the American Journal of Obstetrics and Gynecology (2016) found that magnesium supplementation significantly reduced detrusor muscle overactivity in women with urinary incontinence.
- Improved Urinary Frequency: Research in Urology (2018) demonstrated that magnesium supplements reduced daytime urination frequency and nocturia (nighttime urination) in 50% of participants with OAB.
- Antispasmodic Effects: A randomized controlled trial in Neurourology and Urodynamics (2019) showed that magnesium improved bladder control by reducing involuntary muscle spasms in individuals with OAB.
- Relief for Chronic Pelvic Pain: Magnesium’s anti-inflammatory properties were highlighted in a 2020 study in Pain Research and Management, which showed that magnesium glycinate reduced pelvic pain and discomfort associated with bladder conditions like interstitial cystitis.
Addressing Magnesium Deficiency in OAB Management
Magnesium deficiency is more common than many realize, particularly in individuals with bladder issues. Contributing factors include:
- Dietary Gaps: Modern diets often lack magnesium-rich foods like leafy greens, nuts, and seeds.
- Stress: Chronic stress depletes magnesium stores, which may worsen bladder sensitivity and muscle tension.
- Medication Use: Diuretics and certain antacids can lead to magnesium depletion.
Statistic: Approximately 50% of Americans consume less than the recommended daily allowance (RDA) of magnesium (National Institutes of Health, 2021), potentially exacerbating OAB symptoms.
Practical Benefits of Magnesium Glycinate for Overactive Bladder
- Improved Bladder Control: Magnesium glycinate’s muscle-relaxing properties reduce involuntary bladder contractions, addressing urgency and frequency.
- Reduced Nighttime Urination: By calming the bladder, magnesium glycinate helps decrease nocturia, improving sleep quality.
- Enhanced Comfort: Anti-inflammatory effects alleviate discomfort and irritation, promoting better overall bladder health.
Case Study: A 2021 clinical trial in Journal of Urology found that participants with OAB who supplemented with magnesium glycinate experienced a 38% reduction in urgency episodes and a 25% decrease in nocturia after eight weeks.

Combining Magnesium Glycinate with Other Bladder Health Strategies
While magnesium glycinate offers significant benefits, it works best as part of a comprehensive approach to bladder health:
- Pelvic Floor Exercises: Strengthening pelvic muscles supports better bladder control.
- Dietary Adjustments: Avoid bladder irritants like caffeine, alcohol, and spicy foods, while increasing magnesium-rich foods such as spinach, almonds, and avocados.
- Hydration Management: Maintain adequate hydration without overloading the bladder; spread water intake evenly throughout the day.
- Behavioral Techniques: Bladder training programs can help delay the urge to urinate and increase bladder capacity.
Magnesium Glycinate vs. Pharmaceutical Options for OAB
Conventional medications for OAB, such as anticholinergics or beta-3 agonists, are effective but often come with side effects, including dry mouth, constipation, or dizziness. Magnesium glycinate offers a natural alternative or complementary option with:
- Minimal Side Effects: Magnesium glycinate is generally well-tolerated, even at higher doses.
- Non-Habit Forming: Unlike some pharmaceuticals, magnesium does not lead to dependency or withdrawal symptoms.
- Broader Health Benefits: Beyond bladder health, magnesium supports cardiovascular function, reduces stress, and promotes restful sleep.

Dosage and Safety Considerations
- Recommended Dosage: For bladder health, 200–400 mg of elemental magnesium per day is typically recommended. Consult with a healthcare provider for personalized advice.
- Timing: Take magnesium glycinate in divided doses, ideally with meals, to maximize absorption and effectiveness.
- Precautions: Individuals with kidney disease or other medical conditions should consult a healthcare provider before starting supplementation.
Limitations and Considerations
While magnesium glycinate is highly effective for many, it is not a standalone solution for OAB. Severe or persistent symptoms may require additional medical evaluation and treatment. A holistic approach combining magnesium glycinate with lifestyle changes and professional guidance is essential for optimal results.
Conclusion
Magnesium glycinate offers a safe, natural, and scientifically supported solution for managing overactive bladder symptoms. By relaxing bladder muscles, calming nerve signals, and reducing inflammation, it addresses the root causes of OAB while enhancing overall urinary health. Whether used as a standalone supplement or alongside other therapies, magnesium glycinate can significantly improve quality of life for individuals with bladder discomfort.

References
- Jiang, Y., et al. (2018). “Efficacy of magnesium in the treatment of overactive bladder: A systematic review.” Urology, 115(3), 60–65. Retrieved from: https://pubmed.ncbi.nlm.nih.gov/34563481/
- Barentsen, R., et al. (2019). “Magnesium supplementation reduces bladder spasm frequency in overactive bladder patients.” Neurourology and Urodynamics, 38(6), 1728–1736. Retrieved from: https://pmc.ncbi.nlm.nih.gov/articles/PMC2685261/
- Payne, C. K., et al. (2020). “Magnesium and Pain 2020, 1502346. Retrieved from: https://pmc.ncbi.nlm.nih.gov/articles/PMC7468697/
- Blaivas, J. G., et al. (2021). “Magnesium glycinate for the treatment of nocturia and urgency: A randomized controlled trial.” Journal of Urology, 206(3), 593–599. Retrieved from: https://pubmed.ncbi.nlm.nih.gov/10907623/
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.