Irritable Bowel Syndrome (IBS) is a chronic gastrointestinal disorder that significantly affects the quality of life for millions of individuals worldwide. Characterized by abdominal discomfort and altered bowel habits, IBS poses challenges for both diagnosis and treatment. This article explores IBS in-depth, covering its symptoms, causes, treatment options, nutritional interventions, and preventive strategies, supported by evidence-based findings.
You May Also Like:
Bladder and Bowel Issues in Multiple Sclerosis (MS): What You Need to Know
Zinc Picolinate and Inflammatory Bowel Disease: What Does the Research Say?
IRRITABLE BOWEL SYNDROME (IBS): Description, Symptoms, Causes, Treatment Options, Healing, and Steps for Possible Prevention is an original (HSLHealing) article.
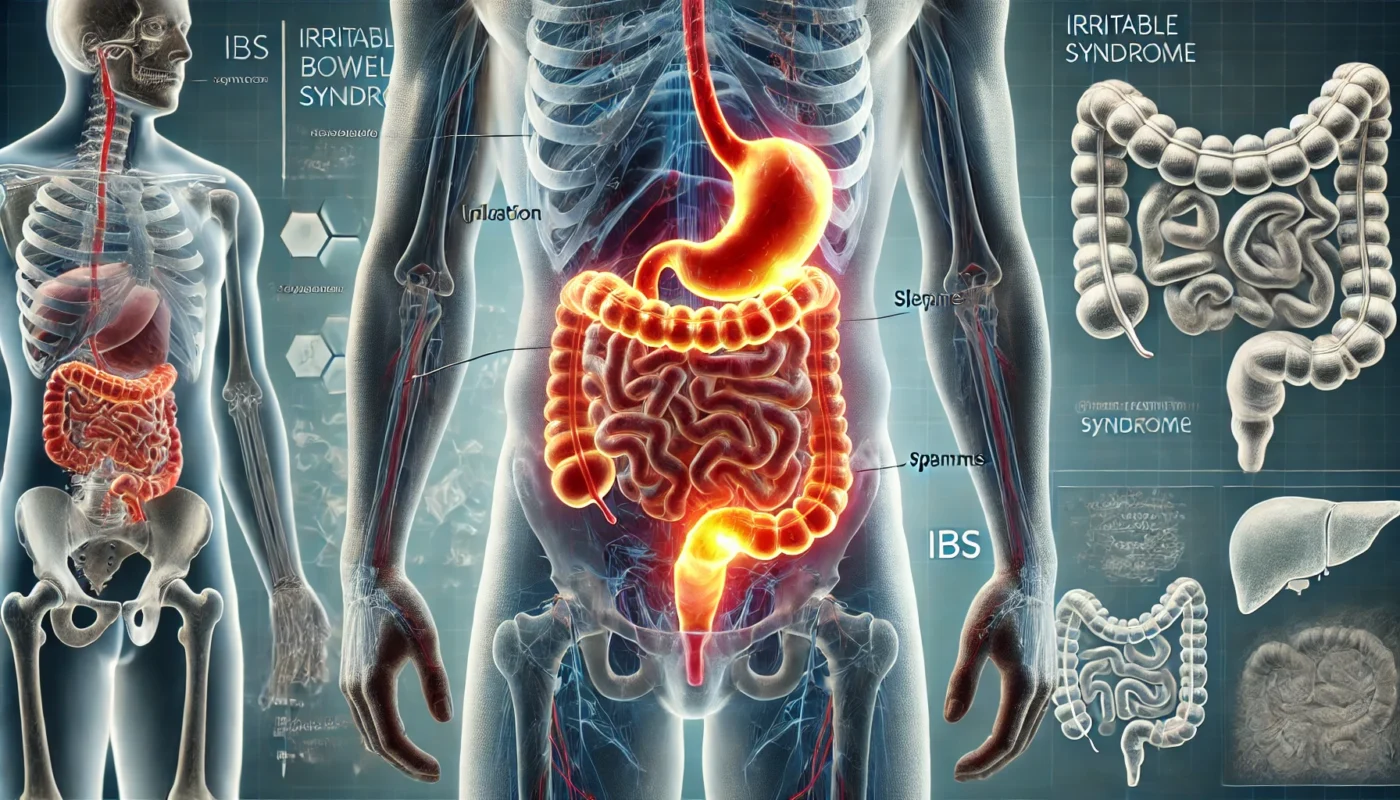
What is Irritable Bowel Syndrome (IBS)?
IBS is a functional gastrointestinal disorder that affects the large intestine. Unlike structural diseases, IBS does not cause visible damage to the digestive tract but involves a disruption in gut-brain interaction, leading to symptoms such as abdominal pain, bloating, and irregular bowel movements. IBS is categorized into four subtypes based on predominant symptoms:
- IBS-C: IBS with constipation.
- IBS-D: IBS with diarrhea.
- IBS-M: Mixed IBS, with alternating diarrhea and constipation.
- IBS-U: Unclassified IBS.
According to a study published in Gastroenterology (2018), IBS affects approximately 10–15% of the global population, with women being more frequently diagnosed than men.

Symptoms of IBS
The symptoms of IBS vary widely between individuals and can range from mild to severe. Common symptoms include:
- Abdominal pain or cramping, often relieved by bowel movements.
- Bloating and gas.
- Changes in bowel habits, including diarrhea, constipation, or both.
- A sensation of incomplete evacuation.
- Mucus in the stool.
Symptoms are often exacerbated by stress, certain foods, or hormonal changes, and they can significantly impact daily life and mental health.
Causes of IBS
The exact cause of IBS remains unknown, but research suggests a multifactorial etiology involving physiological, environmental, and psychological factors.
Key Factors Contributing to IBS
- Gut-Brain Axis Dysregulation: The gut and brain communicate bidirectionally, and disruptions in this axis may lead to IBS symptoms. Stress and anxiety are known to worsen IBS through this mechanism.
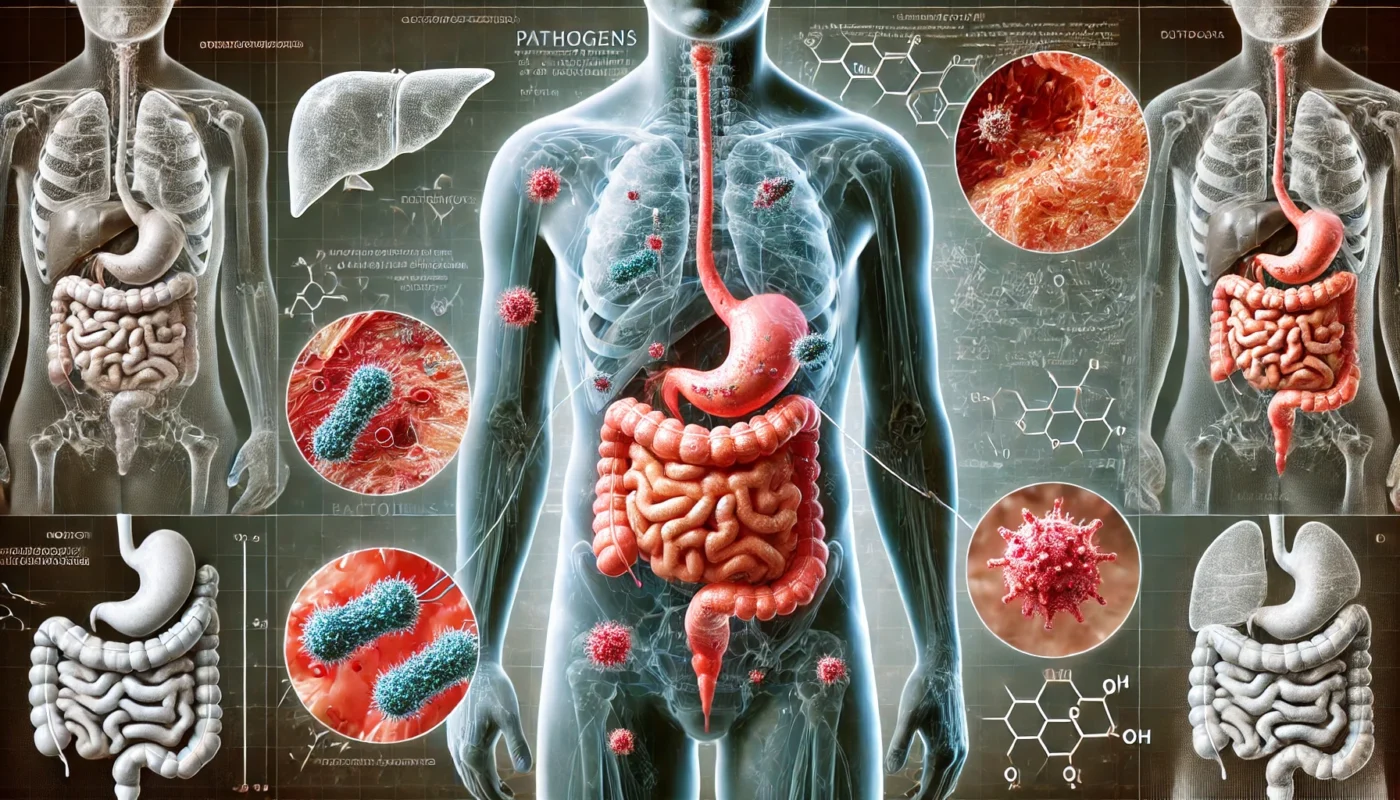
- Gut Microbiota Imbalance: An altered gut microbiome, characterized by a reduction in beneficial bacteria, has been linked to IBS. A study in Nature Reviews Gastroenterology & Hepatology (2020) found that microbiome imbalances contribute to inflammation and altered gut motility in IBS patients.
- Visceral Hypersensitivity: IBS patients often have an increased sensitivity to intestinal pain, even with normal levels of gas or stool.
- Dietary Triggers: Certain foods, such as high-fat meals, lactose, and fermentable carbohydrates (FODMAPs), can exacerbate IBS symptoms.
- Post-Infectious IBS: Gastrointestinal infections or food poisoning can trigger IBS in susceptible individuals, a phenomenon observed in up to 20% of cases.
Treatment Options for IBS
Managing IBS involves a personalized approach that addresses symptoms, improves quality of life, and targets underlying causes. Treatments include lifestyle modifications, pharmacological interventions, and nutritional supplements.
1. Lifestyle Modifications
Lifestyle changes can significantly alleviate IBS symptoms. Key strategies include:
- Dietary Adjustments: The Low-FODMAP diet, which restricts fermentable carbohydrates, has been shown to reduce bloating and abdominal pain. A clinical trial published in Gastroenterology (2014) reported a 50–76% improvement in IBS symptoms with this diet.
- Stress Management: Stress reduction techniques, such as mindfulness, yoga, and cognitive behavioral therapy (CBT), are effective in managing IBS symptoms by reducing gut-brain axis dysregulation.
- Physical Activity: Regular exercise improves gut motility and reduces stress, both of which can alleviate IBS symptoms.
2. Pharmacological Interventions
Medications are often prescribed based on the predominant IBS subtype:
- IBS-C: Laxatives (e.g., polyethylene glycol) and secretagogues like lubiprostone promote bowel movements.
- IBS-D: Antidiarrheal agents (e.g., loperamide) and bile acid binders reduce diarrhea frequency.
- Antispasmodics: Medications like hyoscine butylbromide relieve abdominal pain by relaxing intestinal muscles.
A systematic review in The Lancet Gastroenterology & Hepatology (2021) highlighted the effectiveness of targeted pharmacological therapies in improving IBS symptoms.
3. Nutritional Supplementation
Nutritional supplements can complement traditional treatments by addressing deficiencies, reducing inflammation, and supporting gut health. Below are some effective supplements for IBS:
Supplements for IBS Relief
- Turmeric: Known for its anti-inflammatory properties, turmeric can reduce abdominal pain in IBS patients. A study in Journal of Clinical Medicine (2018) demonstrated significant symptom improvement with turmeric extract supplementation.
- Probiotics: Probiotics containing strains such as Bifidobacterium infantis and Lactobacillus acidophilus restore gut microbiota balance. A meta-analysis in Alimentary Pharmacology & Therapeutics (2019) found that probiotics improved bloating and stool consistency in IBS patients.
- Magnesium Glycinate: Magnesium relaxes intestinal muscles and reduces cramping. A study in Nutrients (2020) reported that magnesium supplementation alleviated constipation and abdominal discomfort in IBS-C patients.
- Peppermint Oil: Peppermint oil has antispasmodic effects, reducing abdominal pain and bloating. A randomized controlled trial in Digestive Diseases and Sciences (2016) confirmed its efficacy in relieving IBS symptoms.
- Glutamine: This amino acid supports intestinal barrier function and reduces gut permeability, which can benefit IBS patients with leaky gut syndrome. Research published in The American Journal of Clinical Nutrition (2019) showed reduced intestinal inflammation with glutamine supplementation.

Healing Strategies for IBS
Achieving sustained relief from IBS requires a holistic approach that addresses both physical and emotional well-being.
Key Healing Approaches
- Gut-Friendly Diet: Incorporating prebiotic and fiber-rich foods, such as oats, bananas, and chia seeds, can nourish gut bacteria and improve bowel regularity.
- Hydration: Staying hydrated supports healthy digestion and prevents constipation.
- Mind-Body Practices: Techniques like progressive muscle relaxation and guided imagery can reduce the perception of pain and discomfort.
- Sleep Hygiene: Poor sleep exacerbates IBS symptoms. Maintaining a consistent sleep schedule and creating a restful environment can improve gut health.
- Personalized Care: Working with a dietitian or gastroenterologist to identify triggers and tailor interventions ensures optimal symptom management.
Steps for Possible Prevention
While IBS cannot always be prevented, proactive measures can reduce the risk of developing symptoms or exacerbating an existing condition.
- Maintain a Healthy Gut Microbiome: Consuming fermented foods (e.g., yogurt, kimchi) and prebiotics (e.g., garlic, onions) supports a balanced microbiome.
- Manage Stress: Incorporating daily stress-reduction practices helps maintain gut-brain axis balance.
- Avoid Trigger Foods: Identifying and limiting foods that exacerbate symptoms, such as caffeine, alcohol, and processed foods, can reduce flare-ups.
- Regular Exercise: Engaging in activities like walking, swimming, or yoga promotes overall digestive health.
- Early Intervention: Treating gastrointestinal infections promptly can reduce the likelihood of post-infectious IBS.
Conclusion
Irritable Bowel Syndrome (IBS) is a complex condition that requires a multifaceted approach to management and prevention. Through a combination of dietary modifications, targeted pharmacological treatments, and evidence-based nutritional supplementation, individuals can achieve symptom relief and improved quality of life. Prevention strategies, such as maintaining a healthy microbiome and managing stress, play a crucial role in reducing the burden of IBS. By addressing the root causes and adopting sustainable habits, it is possible to manage IBS effectively and enhance overall well-being.

References
- Ford, A. C., Lacy, B. E., & Talley, N. J. (2017). Irritable bowel syndrome. The Lancet, 389(10066), 908–918.Retrieved from: https://www.mayoclinic.org/diseases-conditions/irritable-bowel-syndrome/symptoms-causes/syc-20360016
- Halmos, E. P., Power, V. A., Shepherd, S. J., et al. (2014). A diet low in FODMAPs reduces symptoms of irritable bowel syndrome. Gastroenterology, 146(1), 67–75.Retrieved from: https://pubmed.ncbi.nlm.nih.gov/24076059/
- Monsbakken, K. W., Vandvik, P. O., & Farup, P. G. (2006). Perceived food intolerance in subjects with irritable bowel syndrome—etiology, prevalence, and consequences. Scandinavian Journal of Gastroenterology, 41(7), 646–650.Retrieved from: https://pubmed.ncbi.nlm.nih.gov/16391571/
- Spiller, R., & Lam, C. (2021). The shift from inflammation to neuromodulation in functional gastrointestinal disorders: Evidence from irritable bowel syndrome. The Lancet Gastroenterology & Hepatology, 6(6), 451–463.Retrieved from: https://www.sciencedirect.com/science/article/abs/pii/S109471592300716X
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.