Inflammation is a natural and essential part of the body’s immune response. It is the body’s way of signaling the immune system to heal and repair damaged tissue, as well as defend against foreign invaders such as viruses and bacteria. However, chronic inflammation can lead to a host of health issues, including autoimmune diseases, cardiovascular conditions, and metabolic disorders.
You may also like: 20 Powerful Anti-Inflammatory Foods
Acute vs. Chronic Inflammation
Acute inflammation is the body’s immediate response to injury or infection. It is characterized by redness, heat, swelling, and pain and is crucial for healing. Chronic inflammation, on the other hand, is a prolonged inflammatory response that can persist for months or even years. This type of inflammation can result in tissue damage and contribute to diseases such as arthritis, diabetes, and heart disease.
The Role of the Immune System
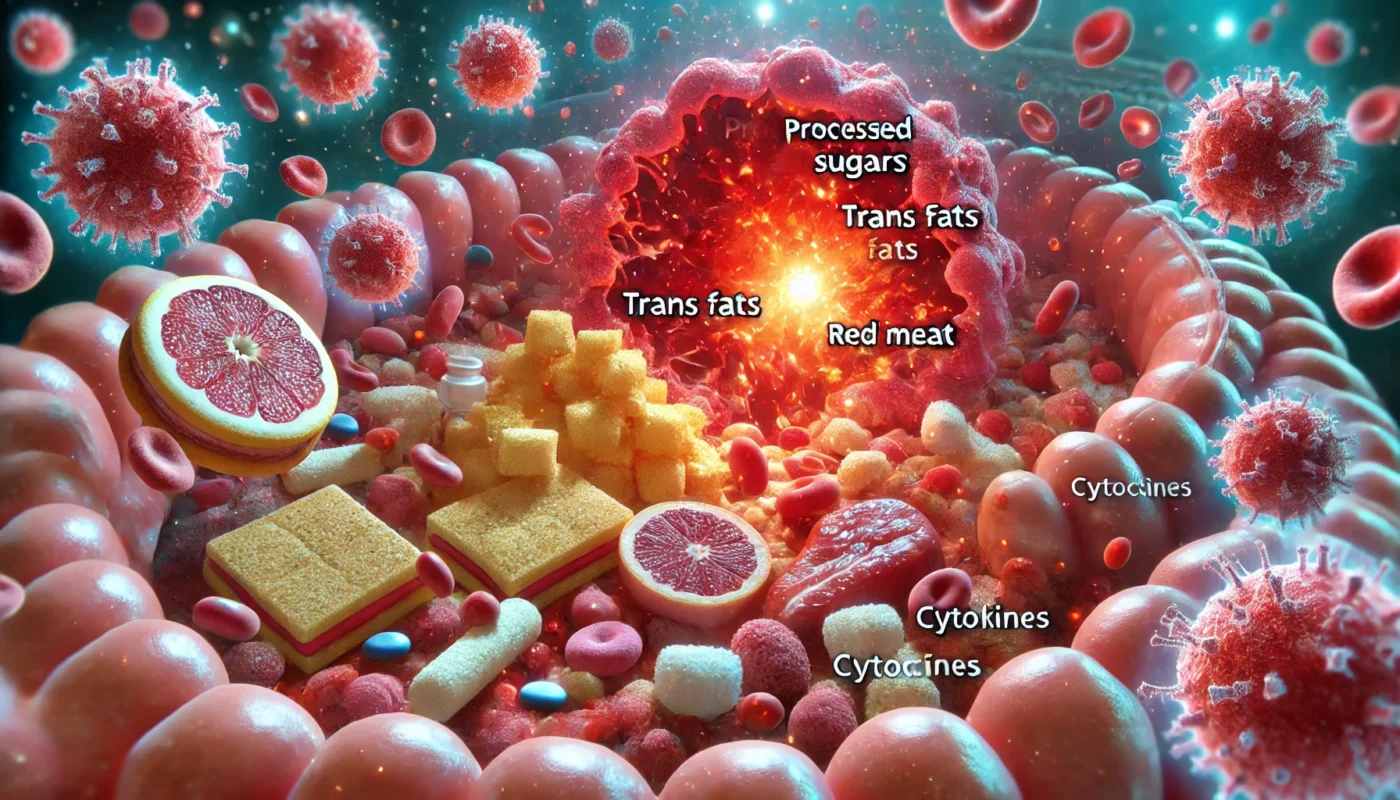
The immune system plays a pivotal role in inflammation. When the body detects harmful stimuli, the immune system responds by releasing white blood cells, cytokines, and other substances to protect the body. While this is beneficial in short-term scenarios, a persistently activated immune system due to chronic inflammation can be detrimental, leading to the aforementioned health conditions.
Inflammation and Disease
Research has established a strong link between chronic inflammation and various diseases. Conditions such as rheumatoid arthritis, inflammatory bowel disease, and even certain cancers have been associated with chronic inflammation. Understanding this connection underscores the importance of managing inflammation through diet and lifestyle choices.
Foods That Contribute to Inflammation
Processed Foods and Sugars
One of the primary culprits in dietary-induced inflammation is processed foods, which are often high in sugars, unhealthy fats, and additives. Excessive sugar consumption, in particular, can lead to increased production of pro-inflammatory cytokines. High-sugar diets have been linked to obesity, insulin resistance, and increased levels of inflammatory markers.
The Science Behind Sugar and Inflammation
The link between sugar and inflammation is well-documented, with studies showing that diets high in added sugars contribute to chronic inflammation and increased risk of chronic disease. Sugars, particularly fructose, can trigger the release of inflammatory compounds and lead to insulin resistance, a precursor to type 2 diabetes and metabolic syndrome.
The Impact of Processed Foods
Processed foods are often loaded with trans fats, preservatives, and artificial ingredients that can fuel inflammation. These foods lack essential nutrients and fiber, which are vital for maintaining a balanced inflammatory response. Consuming a diet high in processed foods is associated with an increased risk of chronic illnesses, including heart disease and obesity.

Alternatives to Processed Sugars
Replacing refined sugars with natural sweeteners like honey, maple syrup, or stevia can help reduce inflammation. Additionally, consuming whole fruits instead of fruit juices or sugary snacks provides fiber and essential nutrients that can combat inflammation.
Red and Processed Meats
Red meats and processed meats, such as sausages and bacon, are often highlighted as pro-inflammatory foods. They contain high levels of saturated fats and advanced glycation end products (AGEs), which can induce inflammation.
Saturated Fats and Their Role
Saturated fats found in red meats can increase levels of LDL cholesterol and promote inflammation. These fats can contribute to the development of atherosclerosis, a condition characterized by the buildup of plaque in arteries, leading to heart disease.
The Effects of Advanced Glycation End Products
AGEs are compounds formed when proteins or fats combine with sugars. These compounds can promote oxidative stress and inflammation in the body. Reducing the intake of AGEs by cooking meats at lower temperatures and opting for lean cuts can help mitigate their inflammatory effects.
Moderation and Alternatives
While not all red meats have the same impact, frequent consumption of processed red meats is associated with an increased inflammatory response. Opting for leaner cuts of meat and incorporating plant-based protein sources like legumes and tofu can help reduce inflammation.
Dairy Products
Dairy, particularly cheese, has been a subject of debate regarding inflammation. Some people may experience inflammation due to lactose intolerance or a sensitivity to casein, a protein found in milk.
Lactose Intolerance and Inflammation
Individuals with lactose intolerance may experience digestive issues and inflammation when consuming dairy products. This occurs when the body lacks the enzyme lactase, necessary for breaking down lactose, leading to gastrointestinal discomfort and inflammation.
Casein Sensitivity and Its Implications
Casein, a protein found in milk, can trigger an immune response in some individuals, leading to inflammation. This is particularly relevant for those with casein sensitivity or allergies, who may experience symptoms ranging from digestive distress to skin rashes.
Dairy Alternatives
For individuals who are sensitive or intolerant, cheese can indeed trigger an inflammatory response. Opting for dairy alternatives such as almond milk, soy yogurt, or lactose-free products can help minimize inflammation while still providing essential nutrients.
Refined Carbohydrates
Refined carbohydrates, such as white bread, pastries, and white rice, can cause inflammation due to their high glycemic index. These foods can lead to spikes in blood sugar levels, which, in turn, can increase inflammatory markers.
The Glycemic Index and Inflammation
Foods with a high glycemic index cause rapid increases in blood sugar levels, prompting an inflammatory response. This is particularly concerning for individuals with insulin resistance or metabolic disorders, as it can exacerbate their condition.
Nutrient Depletion in Refined Carbs
Refined carbohydrates are stripped of their nutritional value and fiber, leading to rapid increases in blood sugar and subsequent inflammation. Whole grains, in contrast, retain their nutrients and fiber, providing a more stable energy source and reducing inflammation.
Choosing Whole Grains
Incorporating whole grains such as quinoa, brown rice, and whole wheat bread into your diet can help stabilize blood sugar levels and reduce inflammation. These grains are rich in fiber and essential nutrients that support a healthy inflammatory response.
Vegetables and Inflammation
Nightshade Vegetables
Certain vegetables, like those in the nightshade family (tomatoes, peppers, eggplants), have been suggested to cause inflammation in some individuals. This is often attributed to the alkaloids present in these plants, which may exacerbate inflammation in sensitive individuals.
Alkaloids and Their Effects
Alkaloids, naturally occurring compounds in nightshade vegetables, can cause adverse reactions in some people. These compounds may interfere with nerve function and promote inflammation, especially in individuals with autoimmune disorders like rheumatoid arthritis.
Individual Sensitivities
Are there vegetables that cause inflammation? For some people, yes. Nightshade vegetables can contribute to inflammation, particularly in those with existing sensitivities or autoimmune conditions. It’s essential to identify personal triggers and adjust dietary choices accordingly.
Exploring Alternatives
For those sensitive to nightshades, exploring alternative vegetables such as leafy greens, cruciferous vegetables, and root vegetables can provide nutritional benefits without triggering inflammation.
Corn and Inflammation
Corn is another food often implicated in inflammatory responses. It is commonly found in processed foods and may contribute to inflammation due to its omega-6 fatty acid content and potential for causing spikes in blood glucose.
The Omega-6 and Omega-3 Balance
A diet high in omega-6 fatty acids, commonly found in corn, can disrupt the balance between omega-6 and omega-3 fatty acids, promoting inflammation. Maintaining a balanced ratio of these fatty acids is crucial for reducing inflammation and supporting overall health.
Corn in Processed Foods
Corn is a staple ingredient in many processed foods, often in the form of high fructose corn syrup or corn oil. These processed forms can contribute to inflammation and should be consumed in moderation.
Moderation and Alternatives
Is corn inflammatory? It can be, particularly when consumed in large quantities or as part of a diet high in processed foods. Opting for organic, non-GMO corn and balancing it with anti-inflammatory foods can help manage its impact on inflammation.
Managing Inflammation Through Diet
Anti-Inflammatory Foods
In contrast to pro-inflammatory foods, there are numerous foods known for their anti-inflammatory properties. These include:
Fruits and Vegetables
Rich in antioxidants and phytonutrients, fruits and vegetables like berries, leafy greens, and cruciferous vegetables can help reduce inflammation. These foods provide essential vitamins and minerals that support the immune system and promote overall health.
Healthy Fats
Omega-3 fatty acids found in fatty fish (salmon, mackerel), flaxseeds, and walnuts are known to combat inflammation. Incorporating these healthy fats into your diet can help balance the inflammatory response and support heart health.
Whole Grains
Unlike refined grains, whole grains such as quinoa, brown rice, and oats have a lower glycemic index and are rich in fiber, which can help reduce inflammation. These grains provide a steady source of energy and support digestive health.
Herbs and Spices
Turmeric, ginger, and garlic are powerful anti-inflammatory agents that can be easily incorporated into meals. These spices have been used for centuries in traditional medicine for their healing properties and can enhance the flavor of dishes while reducing inflammation.
Lifestyle Changes
Apart from dietary adjustments, lifestyle changes can also play a significant role in managing inflammation:
Regular Exercise
Physical activity helps reduce inflammation by lowering levels of pro-inflammatory cytokines and increasing anti-inflammatory substances. Engaging in regular exercise, such as walking, swimming, or yoga, can improve overall health and reduce inflammation.
Stress Management
Chronic stress can lead to increased inflammation, so practices such as meditation, yoga, and deep-breathing exercises can be beneficial. Managing stress effectively can support a balanced inflammatory response and improve mental well-being.
Adequate Sleep
Ensuring sufficient, quality sleep is essential for maintaining a healthy inflammatory response. Poor sleep can disrupt the body’s natural healing processes and exacerbate inflammation, so prioritizing rest is crucial for overall health.

Conclusion
Understanding the inflammatory response to food is crucial for optimizing your health and well-being. By identifying and minimizing the consumption of pro-inflammatory foods while emphasizing anti-inflammatory choices, you can help manage inflammation and reduce the risk of chronic disease. As always, consider consulting with a healthcare provider or nutritionist to tailor dietary choices to your specific needs and health goals.
Taking a holistic approach to diet and lifestyle can significantly impact your overall health and quality of life, empowering you to live with vitality and resilience. Embrace the journey to wellness with informed choices and a balanced perspective on the foods you consume. By prioritizing anti-inflammatory foods and lifestyle habits, you can support your body’s natural defenses and promote long-term health.
Further Reading:
5 Types of Foods That Cause Inflammation
Foods That Definitely Cause Inflammation
anti-inflammatory, inflammation, diet, nutrition, omega-6, omega-3, healthy fats, whole grains, fruits, vegetables, lifestyle changes, exercise, stress management, sleep, chronic disease, wellness, holistic health
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease

