When it comes to the intricate and fascinating process of wound healing, fibroblasts play a pivotal role that often goes unnoticed. These dynamic cells are integral to the repair and regeneration of tissues, working tirelessly behind the scenes to restore the skin’s integrity after an injury. In this article, we’ll delve into the function of fibroblasts, explore their significance in the wound healing process, and provide insights into how they contribute to each phase of healing. By understanding the multifaceted roles of fibroblasts, we gain a deeper appreciation for the complex biological processes that underpin healing.
You may also like: Key Factors in Proliferative Wound Healing
Understanding the Wound Healing Process
Before we dive into the specifics of fibroblasts, it’s essential to comprehend the broader wound healing process. This complex series of events can be divided into four distinct phases: hemostasis, inflammation, proliferation, and maturation. Each phase is characterized by unique cellular and molecular activities that collectively ensure effective healing. A thorough understanding of these phases reveals the strategic orchestration required to achieve complete tissue repair.
Hemostasis: The Initial Response
Hemostasis is the body’s immediate response to injury, focusing on stopping bleeding and stabilizing the wound site. Blood vessels constrict to minimize blood loss, and platelets aggregate to form a clot, effectively sealing the wound. This clot not only prevents further bleeding but also serves as a temporary matrix for incoming cells. The hemostatic plug provides a foundation for the subsequent inflammatory phase by trapping essential growth factors and signaling molecules.
Inflammation: Mobilizing the Defense
Following hemostasis, the inflammatory phase is initiated as the immune system’s response to injury. Immune cells, such as neutrophils and macrophages, are recruited to the wound site to clear debris and pathogens. This phase is marked by redness, swelling, and heat, classic signs of inflammation. These immune cells release cytokines and growth factors, which play a crucial role in attracting fibroblasts and other cells necessary for healing. The inflammatory phase is essential for setting the stage for tissue regeneration, as it cleans the wound bed and prepares it for new tissue formation.
Transition to Proliferation: Preparing the Groundwork
As inflammation subsides, the wound healing process transitions into the proliferation phase. During this phase, fibroblasts become active participants, focusing on tissue formation and repair. The groundwork laid during the hemostasis and inflammation phases ensures that fibroblasts can efficiently execute their functions. Understanding this transition highlights the interconnected nature of the healing phases, where each stage builds upon the previous one to achieve holistic recovery.
Proliferation: Enter the Fibroblasts
The proliferation phase is where fibroblasts truly shine. These cells migrate to the wound site and begin their critical work of rebuilding tissue. Fibroblasts are responsible for producing collagen, a structural protein that forms a scaffold for new tissue formation. This phase also involves angiogenesis, where new blood vessels develop to supply nutrients and oxygen to the healing tissue. By examining this phase more closely, we can appreciate the complexity and coordination required for successful tissue regeneration.
Collagen Production: Building the Scaffold
Fibroblasts’ primary function during the proliferation phase is the synthesis and deposition of collagen. This protein is vital for creating a supportive framework for new tissue, providing both strength and flexibility. Collagen fibers are intricately woven to form a dense network that supports cell attachment and facilitates migration. The structured deposition of collagen is crucial for wound closure, as it helps anchor the newly formed tissue and ensures stability.
Angiogenesis: Fueling the Regeneration
A critical aspect of the proliferation phase is angiogenesis, the formation of new blood vessels from pre-existing ones. Fibroblasts secrete growth factors like VEGF (vascular endothelial growth factor) that stimulate the growth of capillaries. These new blood vessels are essential for delivering oxygen and nutrients to the regenerating tissue, supporting cellular metabolism and energy requirements. Angiogenesis not only sustains fibroblast activity but also aids in the overall healing process by ensuring adequate nourishment for all cells involved.
Granulation Tissue Formation: Laying the Foundation
Granulation tissue, a hallmark of the proliferation phase, consists of newly formed connective tissue and capillaries. Fibroblasts play a pivotal role in its formation by producing the extracellular matrix and collagen. This tissue fills the wound bed, providing a protective environment for further healing. The presence of granulation tissue is a positive indicator of healing progress, as it signifies active cellular and molecular processes working towards complete tissue regeneration.

Maturation: Remodeling the Tissue
In the final stage of wound healing, known as maturation or remodeling, fibroblasts continue to play an essential role. They reorganize the collagen fibers, enhancing the tensile strength of the new tissue. This phase can last for months, resulting in a stronger and more resilient healed area. Delving into the nuances of the maturation phase reveals the long-term commitment of fibroblasts to achieving a fully functional tissue.
Collagen Remodeling: Enhancing Strength
During maturation, fibroblasts focus on reorganizing the collagen fibers into a more structured and aligned pattern. This realignment increases the tensile strength of the tissue, making it more resilient to mechanical stress. Collagen remodeling is a dynamic process that involves the breakdown and reformation of collagen fibers, achieving optimal tissue integrity. Understanding this process underscores the importance of fibroblasts in transitioning from a provisional wound matrix to a fully restored tissue.
Scar Formation: The Visible Outcome
As collagen remodeling progresses, the wound area undergoes changes that may result in scar formation. Fibroblasts play a role in determining the characteristics of the scar by influencing collagen deposition and fiber orientation. While scars are a natural part of the healing process, their appearance can vary based on the balance between collagen production and degradation. Insight into scar formation highlights the delicate balance fibroblasts maintain between rapid healing and functional tissue restoration.
Functional Recovery: Achieving Resilience
The ultimate goal of the maturation phase is to restore the tissue’s function and strength. Fibroblasts, through their remodeling activities, contribute to the restoration of the skin’s barrier function and mechanical properties. Achieving functional recovery involves a delicate interplay of cellular activities and molecular signals, ensuring that the healed tissue can withstand daily challenges. The resilience achieved during maturation reflects the culmination of fibroblast efforts throughout the entire healing process.
The Function of Fibroblasts in Wound Healing
Fibroblasts are multifunctional cells with a range of responsibilities during the healing process. Let’s explore their key functions in greater detail. By examining their diverse roles, we can appreciate the versatility and adaptability of these critical cells.
Collagen Synthesis and Deposition
One of the primary roles of fibroblasts is the synthesis and deposition of collagen, which forms the structural framework of new tissue. Collagen not only provides strength and support but also facilitates cell attachment and migration, essential for effective wound closure. The ability of fibroblasts to modulate collagen production in response to environmental cues demonstrates their adaptability and responsiveness to the wound environment.
Extracellular Matrix Formation
Fibroblasts contribute to the formation of the extracellular matrix (ECM), a complex network of proteins and molecules that provide structural support to cells. The ECM acts as a scaffold for tissue regeneration, guiding cell movement and facilitating communication between cells. The dynamic nature of the ECM, shaped by fibroblast activity, underscores its role as a critical component in orchestrating cellular interactions and promoting healing.
Angiogenesis Support
Fibroblasts secrete various growth factors that promote angiogenesis, ensuring an adequate blood supply to the healing tissue. This is crucial for delivering oxygen and nutrients to the regenerating cells, enhancing the overall healing process. The ability of fibroblasts to influence vascular dynamics highlights their indirect yet vital role in sustaining the metabolic needs of the healing tissue.
Wound Contraction
Fibroblasts also play a role in wound contraction, a process that reduces the size of the wound by pulling the edges together. This occurs through the generation of contractile forces within the fibroblasts, facilitating faster closure of the wound. By understanding wound contraction, we gain insight into the mechanical capabilities of fibroblasts and their contribution to the efficiency of wound resolution.
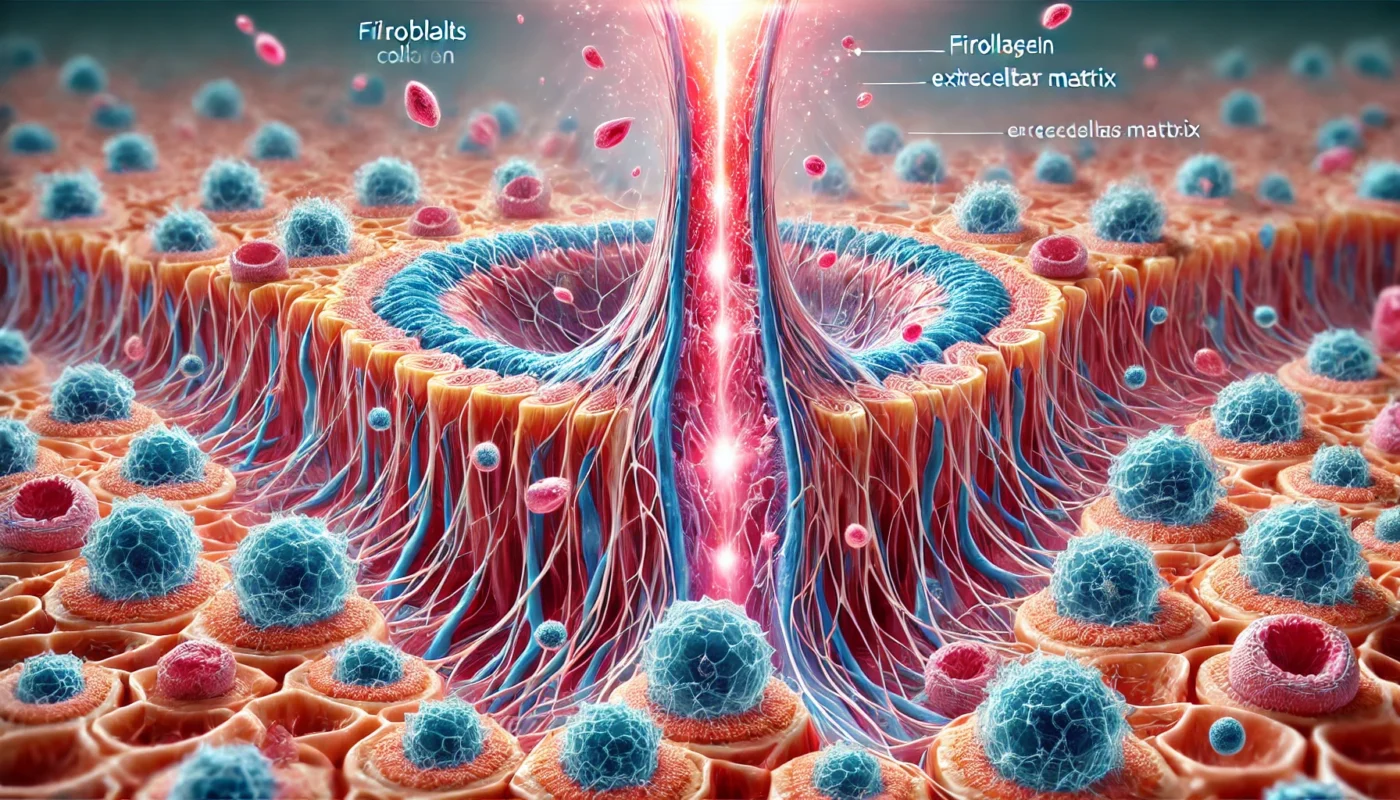
Visualizing the Fibroblastic Phase of Healing
The fibroblastic phase of healing is a dynamic period characterized by rapid cellular activity. Visualizing this phase can provide a better understanding of the complex interactions that occur within the wound environment. Diagrams illustrating fibroblast function and ECM formation can offer valuable insights into the healing process. By visualizing these processes, we can appreciate the intricate choreography of cells and molecules that work in harmony to achieve healing.
Cellular Dynamics: A Closer Look
Visual representations of the fibroblastic phase highlight the diverse cellular activities taking place within the wound. Illustrations can depict fibroblast migration, collagen deposition, and ECM formation, offering a comprehensive view of their interactions. By examining these dynamics, we gain a deeper appreciation for the complexity of the healing process and the precision with which fibroblasts execute their roles.
ECM Architecture: The Structural Blueprint
Visualizing the extracellular matrix during the fibroblastic phase reveals its architectural complexity and significance. Diagrams can showcase the intricate network of proteins and molecules that fibroblasts produce, emphasizing its role as a scaffold for cellular activities. Understanding ECM architecture provides insight into how fibroblasts create an environment conducive to tissue regeneration and healing.
Angiogenesis in Action: Vascular Transformation
Illustrations of angiogenesis during the fibroblastic phase can demonstrate the formation of new blood vessels and their integration into the wound environment. Visual depictions of capillary sprouting and network formation highlight the critical role of fibroblasts in supporting vascular development. By visualizing angiogenesis, we can better appreciate the interconnectedness of cellular activities that sustain the healing process.
Supporting Fibroblast Function Through Nutrition and Lifestyle
To optimize the wound healing process and support fibroblast function, it’s essential to consider nutritional and lifestyle factors that contribute to overall health and wellbeing. By adopting supportive habits, we can enhance the efficiency and effectiveness of fibroblast activity.
Nutritional Support
A well-balanced diet rich in vitamins and minerals is crucial for effective wound healing. Nutrients such as vitamin C, zinc, and protein play a vital role in collagen synthesis and tissue repair. Incorporating foods like citrus fruits, leafy greens, nuts, and lean meats can provide the necessary building blocks for fibroblast activity. By understanding the nutritional requirements of fibroblasts, we can tailor our diets to support optimal healing.
Hydration and Skin Care
Maintaining proper hydration is essential for optimal cell function, including fibroblasts. Adequate water intake supports cellular processes and helps maintain skin elasticity. Additionally, practicing proper wound care and keeping the wound environment moist can enhance fibroblast activity and promote faster healing. Hydration and skin care practices are integral to creating an environment where fibroblasts can thrive and perform their functions efficiently.
Lifestyle Considerations
Healthy lifestyle choices, such as regular exercise and stress management, can positively impact the wound healing process. Physical activity improves circulation, delivering oxygen and nutrients to the tissues, while stress reduction techniques, such as mindfulness and meditation, can boost the immune system’s response to injury. By integrating these practices into daily routines, we can create a holistic approach to supporting fibroblast function and promoting overall healing.
Conclusion: The Unsung Heroes of Healing
Fibroblasts are the unsung heroes of wound healing, orchestrating a complex symphony of cellular activities that lead to tissue repair and regeneration. Understanding their role in the healing process provides valuable insights into how we can support optimal recovery and improve overall health and wellbeing. By nourishing our bodies with the right nutrients, staying hydrated, and embracing healthy lifestyle practices, we can empower fibroblasts to perform their essential functions and facilitate effective wound healing.
Incorporating this knowledge into our daily routines not only enhances our understanding of health and wellness but also empowers us to take charge of our healing journey. Whether you’re a fitness enthusiast, health enthusiast, or medical patient, recognizing the significance of fibroblasts in wound healing can lead to more informed decisions and better outcomes for your overall health. By appreciating the tireless work of fibroblasts, we honor the remarkable processes that restore our bodies and enable us to live healthier, more resilient lives.
Further Reading:
The wound healing process: Factors, speed & phases
General Principles of Wound Healing in Small Animals
fibroblasts, wound healing, cellular dynamics, extracellular matrix, angiogenesis, nutrition, hydration, skin care, lifestyle, tissue repair, collagen synthesis, health and wellness, recovery, fibroblastic phase, wound contraction
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.