Dysmenorrhea, commonly referred to as menstrual cramps, is a medical condition characterized by painful periods that significantly impact daily activities and quality of life. Affecting up to 90% of menstruating women, dysmenorrhea is the leading cause of school and work absenteeism among young women worldwide, according to a review in The Lancet (2020). This article provides an in-depth exploration of dysmenorrhea, including its symptoms, causes, treatment options, and prevention strategies, along with evidence-based nutritional interventions to alleviate symptoms.
You May Also Like:
How Zinc Picolinate Reduces Symptoms of Menstrual Cramps: What Science Reveals
The Role of Magnesium Glycinate in Reducing Pregnancy-Related Cramps
What is Dysmenorrhea?
Dysmenorrhea is categorized into two types:
- Primary Dysmenorrhea: Menstrual pain without an underlying medical condition, typically beginning in adolescence. It is caused by excessive production of prostaglandins, hormone-like substances that trigger uterine contractions.
- Secondary Dysmenorrhea: Menstrual pain associated with underlying reproductive disorders such as endometriosis, adenomyosis, fibroids, or pelvic inflammatory disease.
The severity of dysmenorrhea varies, with some individuals experiencing mild discomfort and others suffering from debilitating pain that interferes with daily activities.

Symptoms of Dysmenorrhea
The hallmark symptom of dysmenorrhea is cramping pain in the lower abdomen, but other symptoms often accompany it:
1. Primary Symptoms:
- Intense, throbbing, or cramping pain in the lower abdomen or pelvis.
- Pain beginning 1–2 days before menstruation and subsiding within 2–3 days of the period’s onset.
2. Associated Symptoms:
- Nausea, vomiting, and diarrhea.
- Fatigue and headache.
- Lower back or thigh pain.
3. In Secondary Dysmenorrhea:
- Symptoms may include irregular menstrual cycles, heavy bleeding, or pain unrelated to menstruation, often linked to underlying conditions like endometriosis.
A study in The Journal of Obstetrics and Gynaecology Research (2021) reported that primary dysmenorrhea is the most prevalent gynecological complaint, affecting 50–70% of women of reproductive age.
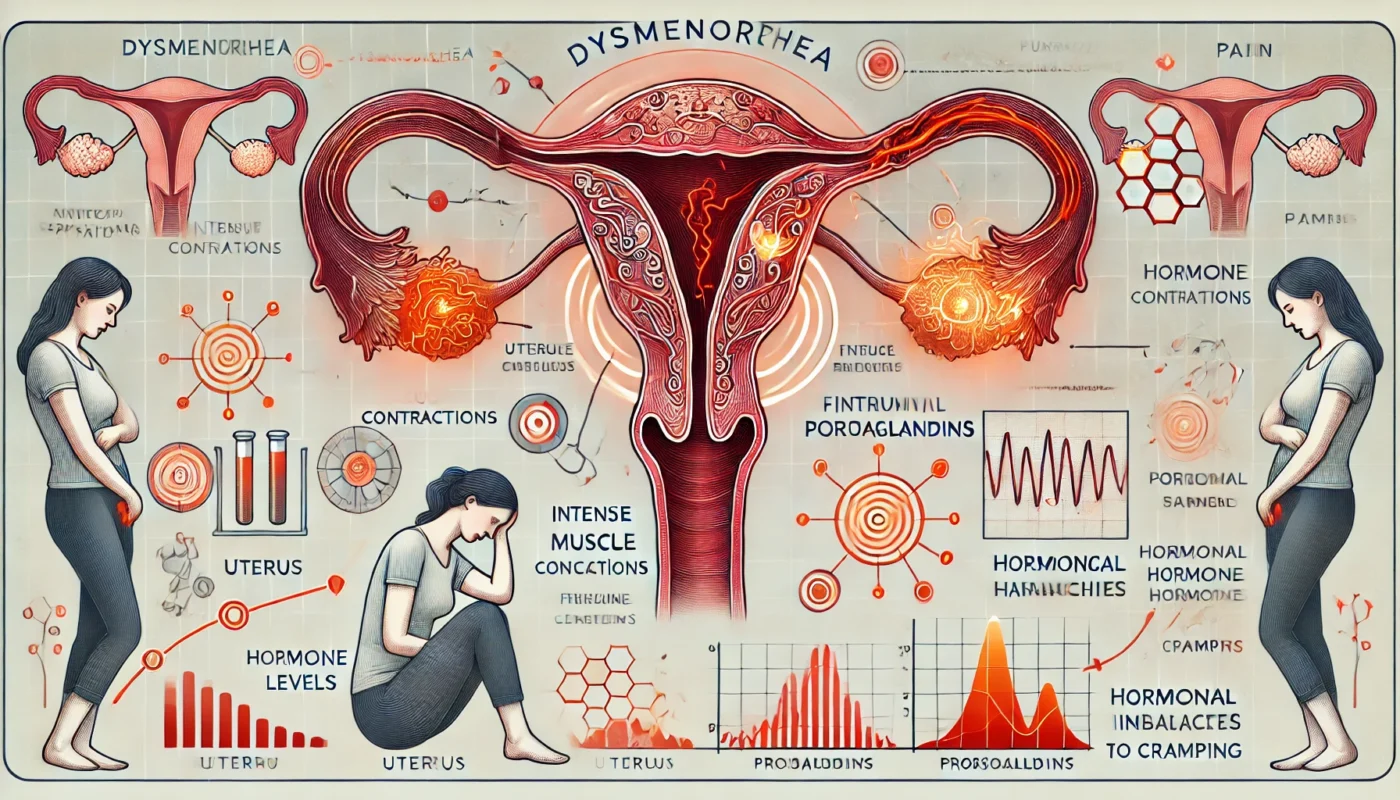
Causes of Dysmenorrhea
The underlying causes of dysmenorrhea differ depending on whether it is primary or secondary:
1. Primary Dysmenorrhea:
- Elevated prostaglandin levels increase the intensity and frequency of uterine contractions, reducing blood flow to the uterus and causing pain.
2. Secondary Dysmenorrhea:
- Endometriosis: Uterine-like tissue grows outside the uterus, causing inflammation and pain.
- Adenomyosis: Endometrial tissue grows into the uterine wall, leading to heavy, painful periods.
- Uterine Fibroids: Noncancerous growths in the uterus can increase menstrual pain.
- Pelvic Inflammatory Disease: Infections in the reproductive organs can cause chronic pelvic pain.
3. Risk Factors:
- Early menarche (onset of menstruation before age 12).
- Family history of dysmenorrhea.
- Smoking, obesity, and lack of physical activity.
Treatment Options for Dysmenorrhea
Effective management of dysmenorrhea involves addressing the symptoms and underlying causes while improving overall quality of life. Treatment options include pharmacological interventions, non-pharmacological therapies, and surgical approaches.
1. Pharmacological Treatments:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): First-line therapy for pain relief, as they reduce prostaglandin production. A study in The Cochrane Database of Systematic Reviews (2021) found that NSAIDs were significantly more effective than placebo in alleviating menstrual pain.
- Hormonal Contraceptives: Regulate ovulation and reduce prostaglandin levels, effectively relieving pain.
- Progestin-Only Medications: Beneficial for individuals with contraindications to estrogen-containing contraceptives.
2. Non-Pharmacological Treatments:
- Heat Therapy: Application of a heating pad to the lower abdomen can relax uterine muscles and reduce pain.
- Acupuncture: A review in Pain Medicine (2020) found that acupuncture reduced pain intensity and improved symptoms in individuals with primary dysmenorrhea.
- Lifestyle Modifications: Regular exercise and stress management can decrease the severity of symptoms.
3. Surgical Interventions:
- Reserved for cases of secondary dysmenorrhea caused by conditions such as endometriosis or fibroids. Procedures include laparoscopic surgery to remove endometrial implants or fibroids.
Nutritional Supplementation for Dysmenorrhea Relief
Nutritional supplements can complement traditional treatments by addressing deficiencies, reducing inflammation, and modulating pain pathways. Evidence-based options include:
- Vitamin E
Vitamin E acts as an antioxidant and reduces the intensity of menstrual cramps. A study published in The Journal of Obstetrics and Gynaecology Research in 2019 found that vitamin E supplementation improved pain relief, particularly when combined with NSAIDs. - Turmeric (Curcumin)
Curcumin, the active compound in turmeric, has powerful anti-inflammatory properties. A clinical trial published in Phytotherapy Research in 2021 found that curcumin supplementation reduced menstrual pain and improved quality of life for individuals with primary dysmenorrhea. - Omega-3 Fatty Acids
Omega-3 fatty acids reduce inflammation and prostaglandin synthesis, alleviating menstrual pain. Research published in Prostaglandins, Leukotrienes, and Essential Fatty Acids in 2020 showed that omega-3 supplementation reduced dysmenorrhea symptoms and decreased the reliance on pain medications. - Magnesium Glycinate
Magnesium promotes muscle relaxation and reduces prostaglandin production, which is associated with menstrual cramps. A randomized controlled trial published in Magnesium Research in 2014 reported that magnesium supplementation significantly reduced the severity of menstrual cramps in individuals with dysmenorrhea. - Ginger
Ginger, known for its anti-inflammatory effects, has been found to be as effective as NSAIDs for pain relief. A clinical trial published in Pain Management in 2020 showed that ginger supplementation significantly reduced menstrual pain in individuals with dysmenorrhea. - Calcium and Vitamin D
Calcium and vitamin D regulate muscle function and reduce menstrual pain. A study published in Clinical Nutrition in 2020 found that supplementation with calcium and vitamin D improved dysmenorrhea symptoms in adolescent girls, making it a valuable option for symptom management.

Healing Strategies for Dysmenorrhea
Healing from dysmenorrhea involves a holistic approach that combines medical treatments, lifestyle modifications, and self-care strategies:
1. Adopt an Anti-Inflammatory Diet:
- Include foods rich in omega-3 fatty acids (salmon, walnuts), antioxidants (berries, leafy greens), and fiber to reduce inflammation.
- Limit processed foods, caffeine, and sugary snacks that may exacerbate symptoms.
2. Incorporate Regular Exercise:
- Moderate physical activity improves blood circulation and reduces the severity of menstrual cramps.
3. Practice Stress Management:
- Stress can worsen dysmenorrhea symptoms. Techniques such as yoga, meditation, and deep breathing promote relaxation.
4. Utilize Heat Therapy:
- Apply heat to the lower abdomen during menstruation to relax uterine muscles and alleviate pain.
5. Monitor Symptoms:
- Keep a menstrual diary to track pain patterns and identify triggers or improvements with specific treatments.
Steps for Possible Prevention
While dysmenorrhea cannot always be prevented, certain lifestyle changes and proactive measures may reduce the risk or severity of symptoms:
1. Maintain a Healthy Lifestyle:
- Regular exercise, a balanced diet, and adequate hydration support overall reproductive health.
2. Avoid Smoking and Alcohol:
- Smoking and excessive alcohol consumption exacerbate inflammation and pain.
3. Address Hormonal Imbalances:
- Regular check-ups and early intervention for hormonal irregularities can prevent the worsening of dysmenorrhea.
4. Use Hormonal Contraceptives as Needed:
- Consult a healthcare provider about hormonal therapies to regulate menstrual cycles and reduce prostaglandin levels.
5. Incorporate Preventive Supplements:
- Nutrients such as magnesium, omega-3 fatty acids, and vitamin E can support long-term menstrual health.
Conclusion
Dysmenorrhea is a common yet often underappreciated condition that can significantly impact the quality of life for menstruating individuals. Through a combination of medical treatments, lifestyle adjustments, and evidence-based nutritional supplementation, dysmenorrhea symptoms can be effectively managed. Supplements such as magnesium glycinate, turmeric, and omega-3 fatty acids provide additional relief by reducing inflammation, relaxing uterine muscles, and modulating pain pathways. By adopting proactive prevention strategies and individualized care, individuals can achieve better menstrual health and improved well-being.

References
- A randomised controlled trial of vitamin E in the treatment of primary dysmenorrhoea. Retrieved from: https://pubmed.ncbi.nlm.nih.gov/15777446/
- Effect of omega-3 fatty acids on intensity of primary dysmenorrhea. Retrieved from: https://pubmed.ncbi.nlm.nih.gov/22261128/
- Magnesium in the gynecological practice: a literature review. Retrieved from: https://pubmed.ncbi.nlm.nih.gov/28392498/
- Dysmenorrhoea and prostaglandins: pharmacological and therapeutic considerations. Retrieved from: https://pubmed.ncbi.nlm.nih.gov/6790261/
- Effect of Curcumin on Dysmenorrhea and Symptoms of Premenstrual Syndrome: A Systematic Review and Meta-Analysis. Retrieved from: https://pmc.ncbi.nlm.nih.gov/articles/PMC10973707/
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.