Diabetes, a chronic condition characterized by elevated blood glucose levels, presents numerous challenges, one of which is impaired wound healing. This complication can lead to severe consequences if not managed properly, making it imperative for individuals with diabetes to understand the nuances of diabetic wound care. This article delves into the intricacies of diabetic wound management and offers practical strategies to prevent complications.
You may also like: Common Causes of Delayed Wound Healing
Understanding the Impact of Diabetes on Wound Healing
The Science Behind Delayed Healing
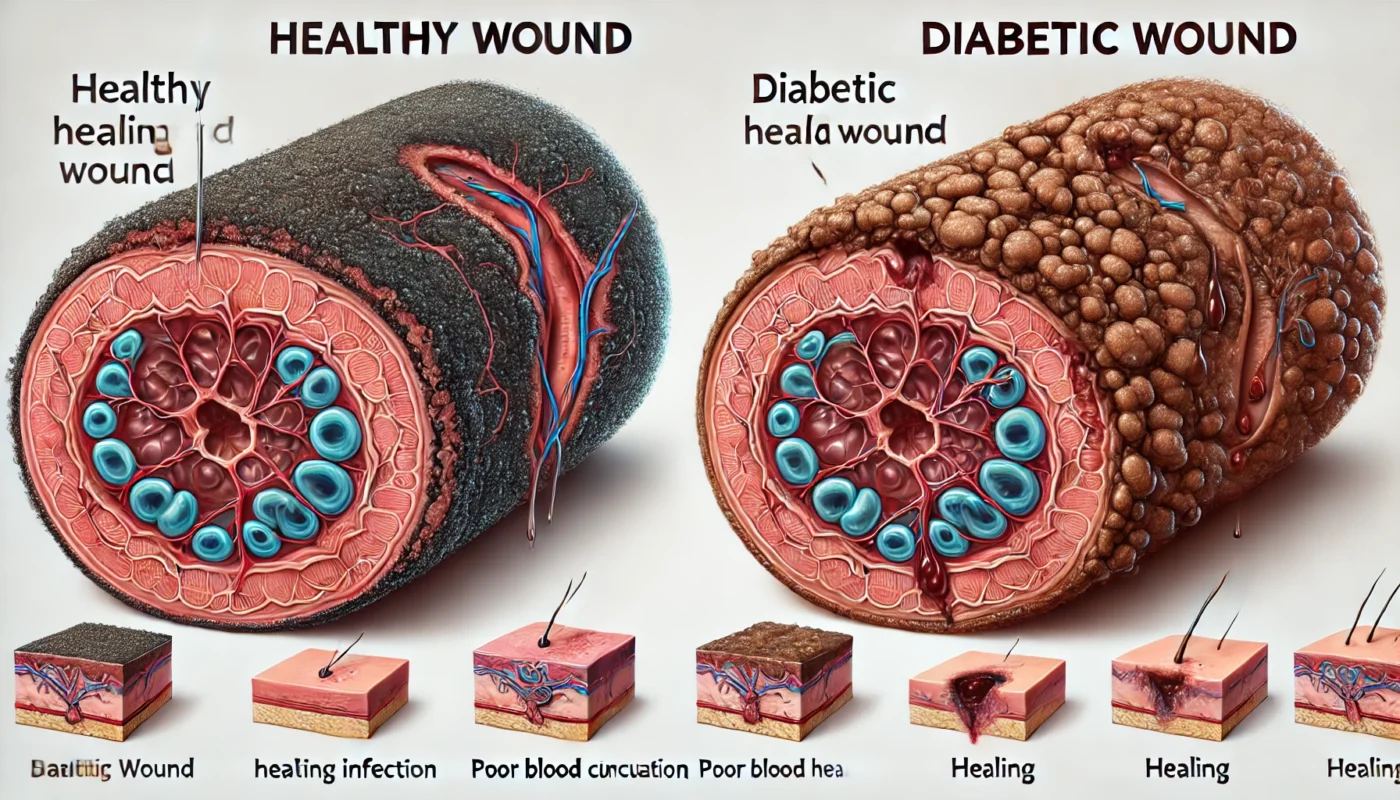
Diabetes affects wound healing by impairing circulation and immune response. High blood sugar levels can damage blood vessels, reducing blood flow to the wound site. This hinders the delivery of essential nutrients and oxygen needed for healing. Moreover, diabetes can compromise immune function, making it difficult for the body to fight infections, a common problem in diabetic wounds.
The reduced blood flow caused by damaged blood vessels means that less oxygen and fewer nutrients reach the site of the wound. This lack of essential elements can significantly slow down the healing process, leaving wounds open and vulnerable to infection for longer periods. Furthermore, high glucose levels can alter cell function, affecting the skin’s ability to repair itself.
Compromised immune function is another critical factor in delayed healing. Diabetics often have a decreased ability to fight off bacteria and other pathogens due to impaired white blood cell function. This weakened immune response can lead to an increased risk of infection, which further complicates and prolongs the wound healing process.
Types of Diabetic Wounds
Diabetic wounds often manifest as ulcers, particularly on the legs and feet. These ulcers can develop from minor cuts or blisters that do not heal properly, leading to serious infections or even amputation if left untreated. Understanding the types of wounds and their development is crucial for effective management.
Foot ulcers are the most common type of diabetic wound, often arising from neuropathy—a loss of sensation due to nerve damage. This makes it easier for injuries to go unnoticed and untreated, allowing them to worsen over time. Leg ulcers, on the other hand, may result from poor circulation and pressure points, often exacerbated by prolonged periods of immobility.
The development of these ulcers can often be traced back to everyday activities. Simple actions such as walking barefoot or wearing ill-fitting shoes can lead to small injuries that, in a diabetic individual, have the potential to evolve into more severe wounds. Vigilance and proactive management are essential to prevent these minor issues from escalating.
Complications Arising from Diabetic Wounds
The complications from diabetic wounds can be severe, leading to infections, gangrene, or even the need for amputation. Infections are particularly dangerous as they can spread rapidly in a body already compromised by diabetes. Gangrene, or tissue death, occurs when blood flow is so severely restricted that it causes tissue to die. This condition often requires surgical intervention, including amputation in severe cases.
The risk of complications underscores the importance of early detection and treatment of wounds. A proactive approach can prevent minor injuries from progressing to a stage where they threaten the individual’s overall health. Understanding the potential complications can motivate individuals to adhere more strictly to prevention and management strategies.
Preventing complications also involves recognizing the signs of worsening wounds. Symptoms such as increased pain, swelling, redness, or discharge should be monitored closely. By being aware of these warning signs, individuals can seek medical attention promptly, potentially averting more serious outcomes.

Prevention Strategies for Diabetic Wounds
Regular Monitoring and Early Detection
Proactive monitoring of any cuts, blisters, or changes in skin condition is vital. Regularly inspect your feet and legs for signs of wounds or infections. Early detection allows for prompt treatment, reducing the risk of complications.
Daily self-examinations are a crucial component of regular monitoring. These examinations should focus on identifying any changes in skin texture, color, or temperature. Using a mirror can help in checking hard-to-see areas, and any abnormalities should be documented and discussed with a healthcare provider.
Incorporating routine check-ups with a healthcare professional can further aid in early detection. These visits provide an opportunity for a thorough examination by a trained eye and can lead to the identification of potential issues before they become significant problems. Regular appointments also allow for the adjustment of treatment plans based on the current state of the individual’s health.
Technology can also play a role in early detection. Wearable devices that monitor foot pressure or temperature changes can alert users to potential issues before they become visible. These innovations, along with traditional monitoring methods, form a comprehensive approach to early detection and prevention.
Maintaining Optimal Blood Sugar Levels
Keeping blood sugar levels within a target range is fundamental in preventing wound complications. Elevated glucose can exacerbate poor circulation and immune function, so adhering to a personalized diabetes management plan is essential.
Diet plays a critical role in maintaining blood sugar levels. A balanced diet rich in whole grains, lean proteins, and vegetables can help stabilize glucose levels. Avoiding high-sugar and high-fat foods is equally important in preventing spikes that can damage blood vessels and impair healing.
Medication adherence is another key aspect of maintaining optimal blood sugar levels. Consistent use of prescribed medications or insulin can prevent dangerous fluctuations in blood glucose. Regular communication with healthcare providers ensures that medication dosages are appropriate and effective.
Lifestyle modifications, such as regular exercise and stress management, complement dietary changes and medication in controlling blood sugar. Physical activity helps the body use insulin more efficiently, while stress reduction techniques can prevent hormone-induced spikes in glucose levels.
Protective Footwear and Skin Care
Wearing appropriate footwear can prevent injuries that lead to wounds. Choose shoes that provide adequate support and cushioning. Additionally, maintain proper skin hygiene by moisturizing regularly to prevent dryness and cracking, which can lead to infections.
Selecting the right footwear involves considering factors such as fit, material, and design. Shoes should fit well without causing pressure points or rubbing that could lead to blisters. Breathable materials are preferable to prevent moisture accumulation, which can promote fungal infections.
In addition to footwear, protective accessories such as socks designed for diabetics can offer additional protection. These socks usually feature seamless designs and are made from materials that wick moisture away from the skin, reducing the risk of irritation and infection.
Skin care routines should include regular washing and moisturizing to maintain skin integrity. Using a gentle cleanser can prevent irritation, while a non-perfumed moisturizer can keep the skin hydrated and flexible. These practices, combined with careful attention to footwear, form a comprehensive approach to preventing wounds.
Advanced Wound Care Techniques
Medical Interventions
For wounds that do not respond to standard care, medical interventions might be necessary. These can include debridement, where dead tissue is removed to promote healing, and specialized dressings that maintain a moist environment conducive to healing.
Debridement is a critical step for wounds with necrotic tissue. The removal of dead tissue not only helps to prevent infection but also encourages the growth of healthy tissue. This procedure can be performed surgically or through less invasive methods, such as using enzymatic ointments.
Specialized dressings can play a significant role in wound care. Options such as hydrocolloid, alginate, or foam dressings help manage exudate and maintain a moist environment, which is crucial for healing. Each dressing type has specific benefits, and the choice depends on the wound’s condition and location.
Wound care may also involve the use of antibiotics or antiseptic solutions to prevent or treat infections. These treatments can be topical or systemic, depending on the severity of the infection. Consulting with a wound care specialist can help determine the most effective treatment plan.
Hyperbaric Oxygen Therapy
Hyperbaric oxygen therapy (HBOT) is an advanced treatment option for chronic diabetic wounds. HBOT involves breathing pure oxygen in a pressurized room, which can enhance oxygen delivery to damaged tissues and accelerate healing.
The pressurized environment of HBOT allows more oxygen to dissolve in the blood, which can promote healing in tissues that are otherwise poorly oxygenated due to impaired circulation. This increased oxygen delivery can help reduce swelling and fight infection, making it a valuable tool for non-healing wounds.
HBOT sessions are typically part of a comprehensive treatment plan and may require multiple visits to achieve optimal results. Each session lasts about one to two hours, and the number of sessions needed varies depending on the severity of the wound and the individual’s response to treatment.
While HBOT is generally safe, it is essential to undergo a thorough evaluation to determine its suitability. Certain conditions, such as respiratory or ear issues, may require adjustments to the treatment protocol to ensure safety and effectiveness.
The Role of Advanced Technology in Wound Care
Innovative technologies are transforming wound care, offering new solutions that complement traditional methods. Devices such as negative pressure wound therapy (NPWT) apply controlled suction to remove fluids and promote healing. This technique can reduce swelling and increase blood flow to the wound site.
Telemedicine is another advancement that enhances wound care by facilitating remote consultations with specialists. Patients can receive guidance on wound management without the need for frequent in-person visits, increasing accessibility and convenience.
Emerging technologies, such as wearable sensors and smart bandages, are also making strides in wound care. These devices monitor wound healing parameters in real-time, providing valuable data that can inform treatment decisions and improve outcomes.

Natural Home Remedies for Diabetic Wounds
Honey and Aloe Vera
Honey, known for its antimicrobial properties, can be applied topically to wounds to help prevent infections. Aloe vera, with its soothing and anti-inflammatory properties, can also be used to promote healing.
Honey, particularly Manuka honey, is renowned for its unique ability to fight bacteria and provide a protective barrier over wounds. Its high sugar content draws moisture away from the wound, creating an environment that inhibits bacterial growth. Applying honey to wounds can reduce inflammation and promote faster healing.
Aloe vera’s anti-inflammatory and moisturizing properties make it an excellent addition to wound care. The gel from the aloe vera plant can soothe irritated skin and reduce swelling, while also providing a natural barrier against infection. Its application can enhance the healing process and improve skin integrity.
Combining honey and aloe vera can create a potent natural remedy for diabetic wounds. The antimicrobial effects of honey complement the soothing properties of aloe vera, offering a holistic approach to wound care that can be used alongside conventional treatments.
Turmeric and Tea Tree Oil
Turmeric contains curcumin, a compound with anti-inflammatory and antimicrobial effects, which can aid in wound healing. Tea tree oil is another natural antiseptic that can help prevent infections when applied to wounds.
Curcumin’s anti-inflammatory properties help reduce swelling and promote healing by modulating the body’s response to injury. Turmeric can be applied as a paste directly to the wound or taken as a supplement to support overall health and healing.
Tea tree oil’s antiseptic properties make it effective in preventing and treating minor infections. Its application should be done with care, as it can cause irritation if used in high concentrations. Diluting tea tree oil with a carrier oil, such as coconut or olive oil, can help mitigate this risk.
Using turmeric and tea tree oil together can create a comprehensive natural remedy. The combination of anti-inflammatory and antiseptic properties can address multiple aspects of wound care, supporting the body’s natural healing processes while preventing infections.
Balanced Nutrition
A diet rich in vitamins and minerals is crucial for wound healing. Ensure adequate intake of vitamin C, zinc, and protein to support tissue repair and immune function. Incorporating a variety of fruits, vegetables, lean proteins, and whole grains can provide the necessary nutrients for optimal healing.
Vitamin C plays a vital role in collagen synthesis, which is essential for wound healing. Consuming foods high in vitamin C, such as citrus fruits, strawberries, and bell peppers, can enhance tissue repair and strengthen the immune system.
Zinc is another critical nutrient that supports wound healing by promoting cell growth and immune function. Foods such as nuts, seeds, and lean meats are excellent sources of zinc and can be easily incorporated into a balanced diet.
Protein is fundamental for repairing damaged tissues and supporting overall healing. Lean meats, beans, and legumes provide high-quality protein that can aid in recovery. A balanced diet that includes these nutrients can enhance the body’s ability to heal and prevent complications.
The Role of Exercise in Wound Management
Enhancing Circulation
Regular physical activity can improve circulation, which is essential for wound healing. Exercises like walking, swimming, or cycling can enhance blood flow and aid in glucose regulation, both of which contribute to faster healing.
Improved circulation ensures that more oxygen and nutrients are delivered to wound sites, supporting the body’s natural healing processes. Engaging in low-impact activities such as walking or swimming can gently boost circulation without putting excessive pressure on the body.
Exercise also helps regulate glucose levels by increasing insulin sensitivity. This regulation is crucial for individuals with diabetes, as stable glucose levels prevent further complications and support overall health. Consistent physical activity is a cornerstone of effective wound management.
Incorporating exercise into daily routines can be as simple as taking short walks after meals or participating in a community fitness class. The key is to find enjoyable activities that encourage regular participation, promoting both physical health and wound healing.
Stress Reduction and Immune Support
Exercise also plays a role in reducing stress and boosting immune function. Lower stress levels can positively impact blood sugar control and, consequently, wound healing.
Physical activity stimulates the release of endorphins, which are natural mood enhancers that reduce stress and promote a sense of well-being. This reduction in stress can lead to better blood sugar control, as stress hormones like cortisol can cause glucose levels to rise.
A strong immune system is vital for preventing infections and supporting wound healing. Regular exercise has been shown to enhance immune function, making the body more resilient to infections and other health challenges. This immune boost can be particularly beneficial for individuals managing chronic conditions like diabetes.
Incorporating relaxation techniques, such as yoga or meditation, can complement physical exercise by further reducing stress and enhancing overall well-being. These practices, combined with regular activity, create a holistic approach to managing diabetes and promoting wound healing.
Building a Sustainable Exercise Routine
Creating a sustainable exercise routine involves setting realistic goals and gradually increasing activity levels. Starting with manageable activities, such as short walks or gentle stretching, can build confidence and establish a foundation for more intense exercise.
Listening to the body and adjusting activities based on individual needs and limitations is crucial. Consulting with a healthcare provider or fitness professional can provide guidance on designing a safe and effective exercise plan tailored to personal health goals.
Maintaining motivation is key to sustaining an exercise routine. Finding activities that are enjoyable and engaging can encourage consistency, while setting achievable milestones provides a sense of accomplishment and progress.
When to Seek Professional Help
Signs of Infection
It’s crucial to recognize signs of infection, such as increased redness, swelling, warmth, or pus. If any of these symptoms are present, seek medical attention promptly to prevent further complications.
Recognizing these signs early can prevent the spread of infection and reduce the risk of more severe outcomes. Prompt medical intervention can lead to more effective treatment, minimizing the potential for complications and promoting quicker recovery.
Understanding the body’s normal healing process can help distinguish between typical wound healing and signs of infection. Any sudden changes in the wound’s appearance or sensation should be taken seriously and evaluated by a healthcare professional.
In addition to visual signs, systemic symptoms such as fever or increased fatigue may indicate an infection. These symptoms should be monitored closely, and medical advice should be sought if they persist or worsen.
Persistent Non-healing Wounds
If a wound does not show signs of healing within a reasonable timeframe, it’s important to consult a healthcare provider. They can assess the wound and recommend appropriate treatments, which may include more aggressive interventions.
Non-healing wounds may require specialized care, such as advanced dressings or surgical interventions, to promote healing. A healthcare provider can perform a thorough evaluation to determine the underlying causes of delayed healing and develop a targeted treatment plan.
Factors such as poor circulation, infection, or inadequate nutrition can contribute to non-healing wounds. Addressing these issues through a comprehensive approach can enhance healing and prevent further complications.
Regular follow-up appointments with healthcare providers ensure that the treatment plan is effective and allows for adjustments as needed. These check-ins provide an opportunity to monitor progress and make necessary changes to optimize outcomes.
The Importance of Professional Guidance
Professional guidance is essential in managing diabetic wounds effectively. Healthcare providers offer expertise in wound care and can recommend treatments tailored to individual needs. Their support is crucial in preventing complications and promoting successful healing.
Developing a trusting relationship with healthcare providers encourages open communication and collaboration. Patients who feel comfortable discussing their concerns and experiences are more likely to receive care that addresses their unique needs and preferences.
Access to specialized wound care services, such as those offered by podiatrists or wound care clinics, can provide additional support and resources. These services often include advanced diagnostic tools and treatment options that enhance the overall management of diabetic wounds.
Conclusion
Managing diabetic wounds effectively requires a comprehensive approach that combines medical interventions, preventive measures, and natural remedies. By understanding how diabetes affects wound healing and implementing these strategies, individuals can significantly reduce the risk of complications and promote faster recovery. Regular communication with healthcare providers and adherence to a diabetes management plan are essential components of successful wound care.
Empowering individuals with knowledge about wound care and diabetes management fosters proactive behavior and informed decision-making. This empowerment leads to better health outcomes and a higher quality of life for those living with diabetes.
Continuous education and awareness about the latest advancements in wound care and diabetes management can further enhance the ability to prevent and treat complications. Staying informed and adaptable to new strategies and technologies is key to achieving optimal wound healing and overall health.
Collaboration between individuals, healthcare providers, and support networks creates a supportive environment for managing diabetes and its associated challenges. This collective effort ensures that individuals have the resources and guidance needed to navigate their health journey successfully.
Further Reading:
Why Is Wound Healing Slower with Diabetes?
Updates in Diabetic Wound Healing, Inflammation, and Scarring
Vitamin C, wound healing, zinc, protein, exercise, circulation, stress reduction, immune support, diabetes management, professional guidance, infection signs, non-healing wounds, healthcare providers, nutrition, holistic approach, diabetic wounds, recovery, health outcomes, tissue repair, physical activity
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.