In the aftermath of any traumatic injury, including stab wounds, the journey to full recovery doesn’t end once the wound has closed. The long-term care of healed stab wounds is a crucial step to ensure optimal recovery and prevent potential complications. This article delves into the complexities of wound healing, offering practical advice and insights grounded in scientific research to help individuals manage their recovery process effectively.
You may also like: Key Factors in Proliferative Wound Healing
Understanding Wound Healing
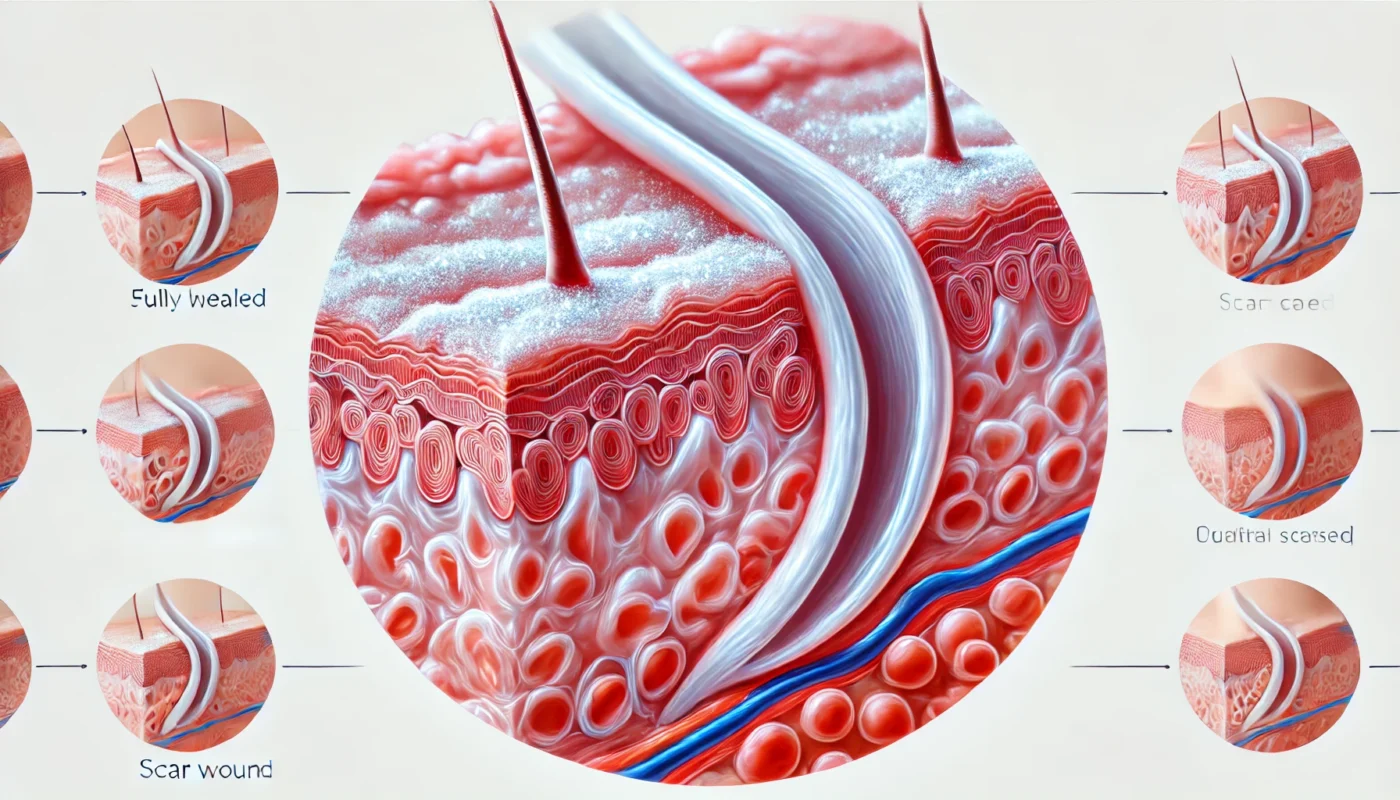
Before diving into long-term care, it’s essential to understand the phases of wound healing. Typically, a stab wound undergoes several stages that each play a vital role in recovery:
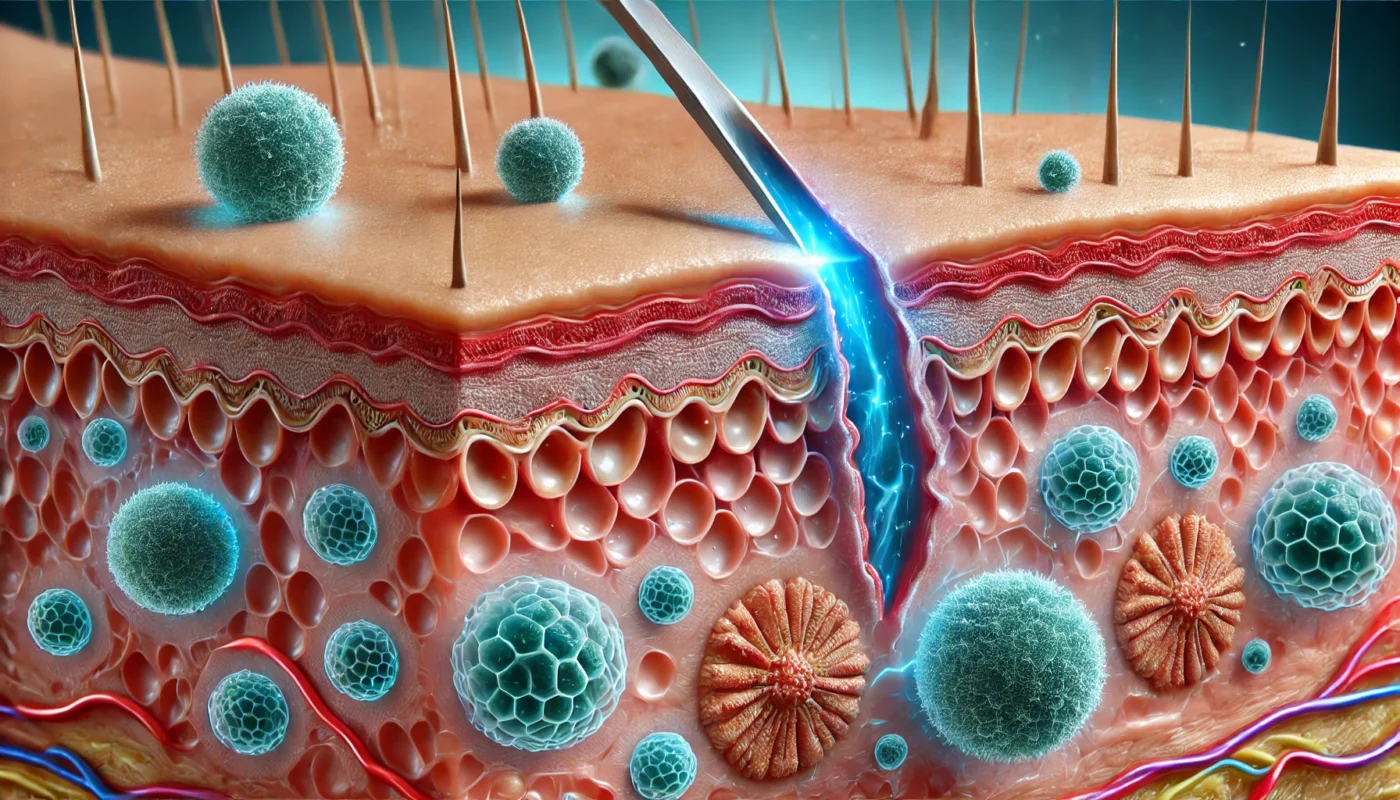
Hemostasis and Inflammation
Immediately after the injury, the body initiates the hemostasis process to stop bleeding. Blood vessels constrict, and clotting factors work to form a clot, which acts as a barrier to infection. This process is crucial as it stabilizes the wound site and prepares it for healing. Concurrently, inflammation occurs as white blood cells move to the area to fend off potential pathogens. This phase, lasting a few days to a week, is marked by redness, heat, and swelling, all of which are natural responses necessary for healing.
Proliferation
The proliferation phase involves the rebuilding of tissue and the formation of new blood vessels, a process known as angiogenesis. Fibroblasts play a key role by synthesizing collagen, which is essential for tissue strength and integrity. As the wound fills with granulation tissue, new epithelial cells form over the wound, providing a protective layer. This phase, which can span several weeks, is vital for restoring the wound’s structure and function.
Maturation or Remodeling
During the maturation phase, the wound undergoes a transformation to increase its tensile strength. Collagen fibers reorganize and become more aligned, leading to a reduction in scar thickness. This phase can last from several months to a year, highlighting the importance of ongoing care even after the wound appears healed. It’s during this time that interventions for scar management and flexibility can have significant impacts on the final appearance and functionality of the healed area.
How Long Do Stab Wounds Take to Heal?
The healing time for stab wounds can vary significantly depending on several factors, including the severity of the wound, its location, and the individual’s overall health. Understanding these aspects can help set realistic expectations and guide effective care strategies.
Depth and Size of the Wound
Deeper and larger wounds naturally require more time to heal due to the greater amount of tissue damage. The depth affects not only the time needed for tissue repair but also the potential for complications such as infections or damage to underlying structures. Patients should be aware that larger wounds may also result in more prominent scarring, which can necessitate additional care and treatment.
Wound Location
The location of the wound plays a critical role in healing time. Areas with more muscle movement, such as joints or places subject to frequent stretching, might heal slower due to the constant tension placed on the wound. Additionally, wounds in areas with limited blood supply, like certain regions of the legs, might experience delayed healing. Understanding the impact of wound location can help in designing a care plan that minimizes movement and stress on the healing area.
Individual Health Factors
A person’s overall health significantly influences wound healing. Factors such as nutrition, underlying medical conditions, and lifestyle choices like smoking can either expedite or impede recovery. Nutritional deficiencies, particularly in vitamins and minerals critical for wound healing, can slow the process. Conditions such as diabetes or circulatory issues can also lead to complications, necessitating more vigilant monitoring and care.
Long-Term Care Strategies
Once a stab wound has healed, there are several strategies to ensure long-term health and minimize scarring. Implementing these strategies can enhance recovery outcomes and improve quality of life.
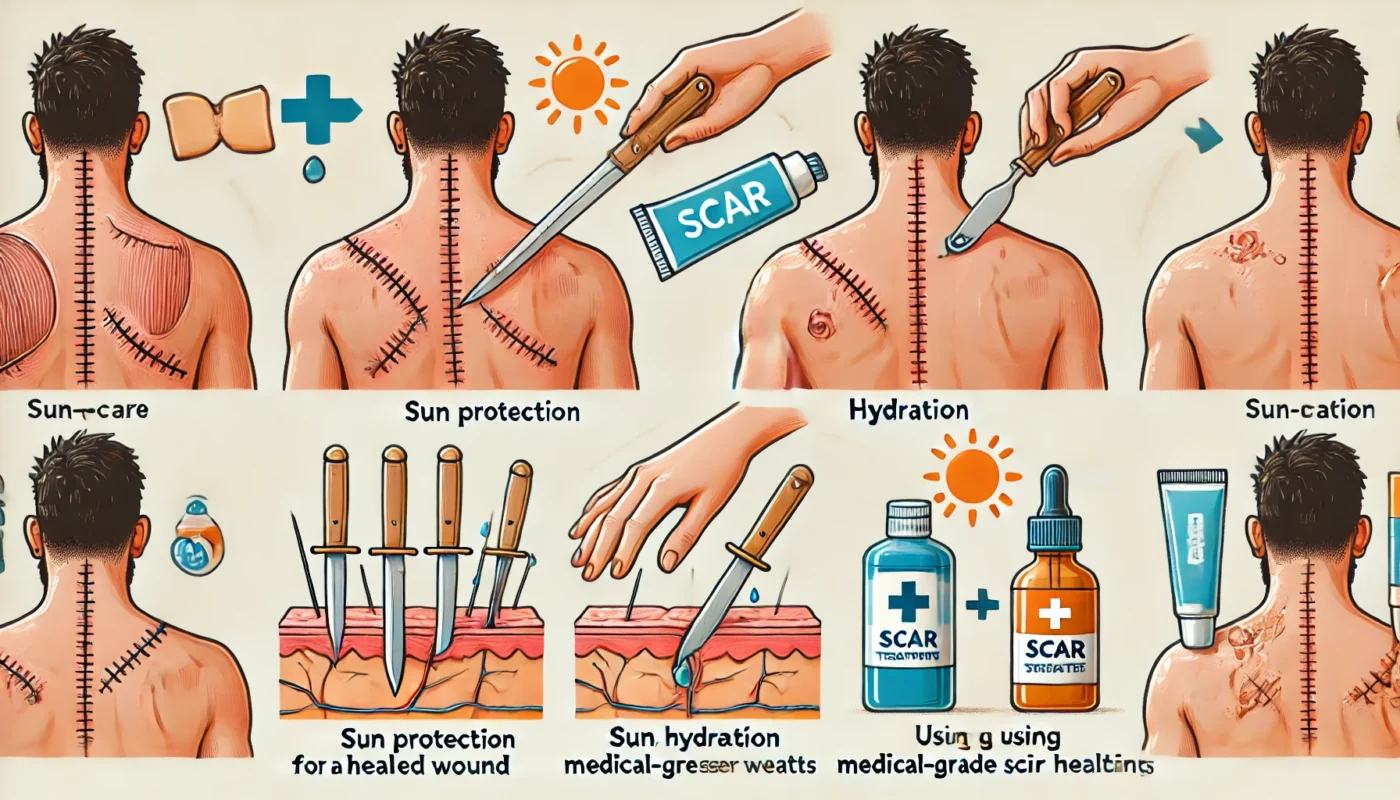
Scar Management
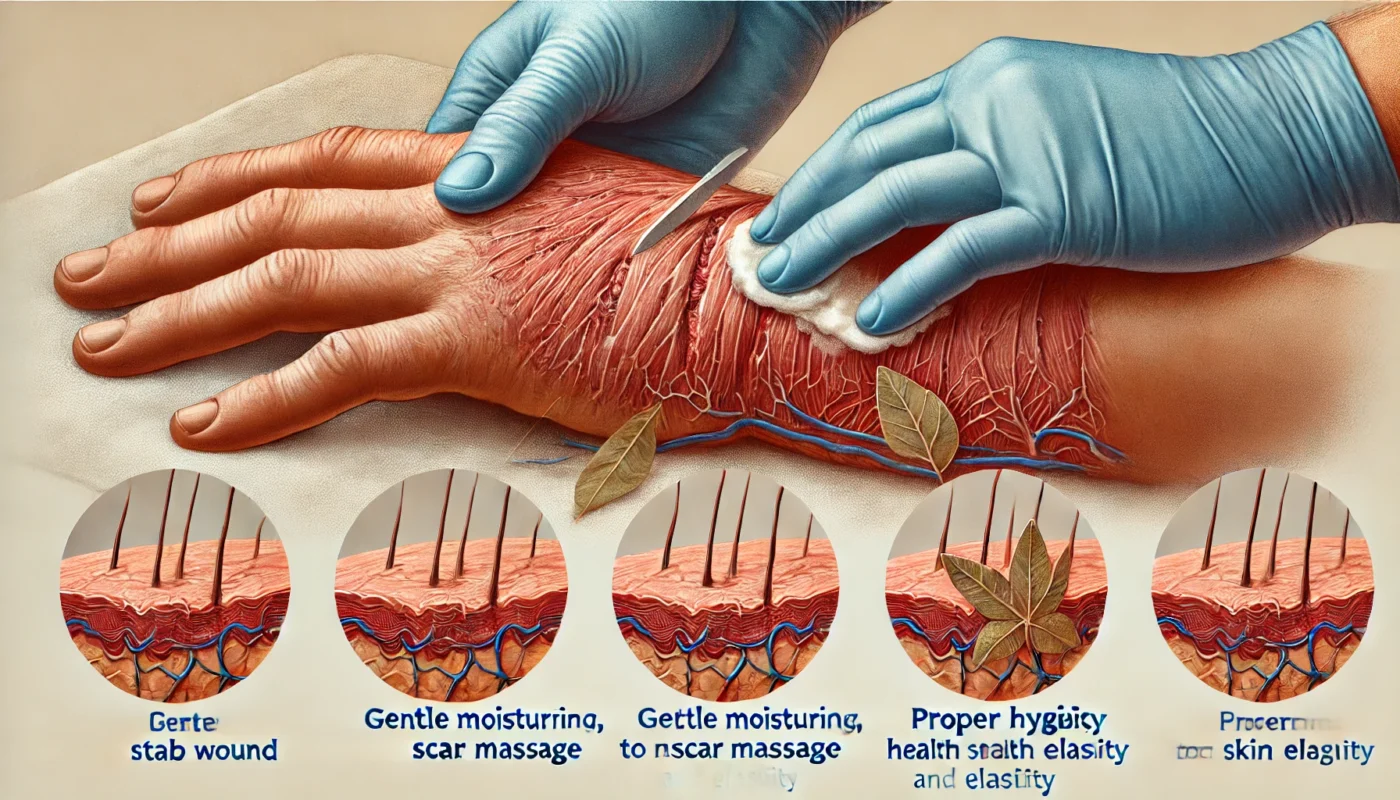
Scar tissue is a natural part of the healing process, but there are ways to manage its appearance and flexibility:
Moisturization
Keeping the scar moisturized is crucial for maintaining its flexibility and improving its appearance. Products like silicone gels and sheets have been shown to be effective in reducing scar thickness and enhancing the skin’s texture. Regular application of moisturizers can also alleviate itching and discomfort often associated with new scar tissue.
Massage Therapy
Gently massaging the scar tissue can help break down fibrous tissue and improve circulation. This practice can increase the elasticity of the skin and reduce the feeling of tightness. Massaging should be done with care to avoid causing damage, and techniques can be learned from a physical therapist or healthcare professional to ensure effectiveness and safety.
Sun Protection
Protecting the scar from UV exposure is essential to prevent hyperpigmentation and ensure even skin tone. Scars are particularly sensitive to sunlight, and UV rays can darken the scar tissue, making it more noticeable. Using broad-spectrum sunscreen or covering the scar with clothing can safeguard against these effects and promote a more uniform healing process.
Exercise and Movement
Regular movement and exercises tailored to the wound’s location can prevent stiffness and improve mobility. However, it’s crucial to consult with a healthcare provider or physiotherapist to design a safe exercise plan.
Tailored Exercise Programs
Designing an exercise program specific to the wound’s location helps in regaining strength and flexibility without compromising healing. Such programs often include gentle stretching and strengthening exercises that are gradually intensified as healing progresses. A professional can help balance the need for movement with the necessity of protecting the healing tissue.
Preventing Stiffness
Incorporating movement into daily routines can prevent stiffness, particularly in areas like joints, where immobility can lead to decreased range of motion. Simple activities, such as walking or light stretching, can contribute to maintaining flexibility. This approach ensures that the surrounding muscles and tissues remain active, supporting overall recovery.
Monitoring Progress
Regular assessment of movement and flexibility can help track progress and adjust exercises as needed. Keeping a log of activities and any discomfort experienced can provide valuable insights into the healing process. This practice also facilitates communication with healthcare providers, enabling timely interventions if issues arise.
Nutrition and Supplements
A balanced diet rich in vitamins and minerals supports the body’s healing processes. Key nutrients include:
Vitamin C
Vitamin C is essential for collagen synthesis, which is crucial for wound healing. It plays a significant role in the formation of new tissue and the repair of damaged cells. Including foods rich in vitamin C, such as citrus fruits, berries, and leafy greens, can enhance the body’s ability to recover effectively.
Zinc
Zinc plays a critical role in cell proliferation and immune function, both vital for wound healing. This mineral supports the repair of damaged tissues and the maintenance of skin integrity. Foods like meat, shellfish, and legumes are excellent sources of zinc and should be included in a healing diet.
Omega-3 Fatty Acids
Found in fish oils, omega-3 fatty acids have anti-inflammatory properties that can aid in healing. These healthy fats help reduce swelling and promote faster recovery. Including sources of omega-3s, such as salmon, walnuts, and flaxseeds, can support the body’s natural healing processes.
Holistic Approaches
Incorporating holistic practices can complement traditional healing methods:
Acupuncture
Some studies suggest acupuncture can enhance circulation and reduce pain in healed wound areas. This ancient practice may help alleviate discomfort and promote relaxation, contributing to overall well-being. Acupuncture should be performed by a licensed practitioner to ensure safety and effectiveness.
Herbal Remedies
Certain herbs, like calendula, are known for their skin-healing properties and can be used as adjuncts to conventional care. Herbal ointments and creams can soothe irritated skin and promote healing. Consulting with a healthcare provider before using herbal remedies ensures they complement other treatments effectively.
Mind-Body Techniques
Practices such as meditation and yoga can support mental and emotional well-being during the recovery process. These techniques help manage stress, which can negatively impact healing if left unchecked. Incorporating regular mind-body practices can enhance overall recovery by promoting a sense of calm and balance.
Can You Take a Shower 24 Hours After a Puncture Wound?
The question of when to shower after a puncture or stab wound is common. Generally, it’s advisable to avoid soaking the wound in water for at least 24 to 48 hours to prevent infection. However, a quick, gentle shower, ensuring the wound area is covered and protected, is often permissible. Always follow your healthcare provider’s specific advice regarding wound care.
Protecting the Wound
When showering, it’s crucial to keep the wound covered with a waterproof bandage to prevent water from entering and causing infection. This precaution helps maintain the sterility of the wound site, reducing the risk of complications. After the shower, gently pat the area dry to avoid disturbing the healing tissue.
Bathing Alternatives
For individuals concerned about wound exposure, sponge baths can be a suitable alternative. Using a damp cloth to clean areas around the wound can help maintain hygiene while protecting the healing site. This method minimizes the risk of water exposure and ensures that the wound remains dry and clean.
Consulting Healthcare Providers
Each wound is unique, and healthcare providers can offer tailored advice on bathing and wound care. Following their recommendations ensures that the wound receives the best care possible, reducing the likelihood of infection or delayed healing. Regular check-ins with a healthcare professional can provide reassurance and guidance throughout the healing process.
Monitoring for Complications
Even after a stab wound has healed, it’s essential to monitor for any signs of complications, such as:
Persistent Pain or Swelling
Persistent pain or swelling could indicate underlying issues like infection or improper healing. It’s important to pay attention to any discomfort that doesn’t subside or worsens over time. Seeking medical evaluation promptly can help address these issues before they lead to more significant problems.
Changes in Sensation
Numbness or tingling around the healed wound might suggest nerve damage. These sensations can impact the functionality of the affected area and should be assessed by a healthcare provider. Early detection and intervention can prevent long-term complications and promote nerve recovery.
Unusual Discharge or Redness
Signs of infection, such as unusual discharge or redness, require immediate medical attention. These symptoms might indicate that bacteria have entered the wound, necessitating treatment to prevent further complications. Monitoring the wound for changes and responding quickly can ensure a swift and effective resolution.
Conclusion
The journey to recovery from a stab wound extends far beyond the initial healing phase. By understanding the intricacies of wound healing and implementing comprehensive long-term care strategies, you can optimize your recovery and minimize complications. Always consult healthcare professionals when creating a care plan and remain attentive to any changes in your condition. With informed care and attention, you can ensure that your recovery process is as smooth and effective as possible, paving the way for a return to normal activities and a healthy future.
Further Reading:
omega-3 fatty acids, healing, holistic approaches, acupuncture, herbal remedies, mind-body techniques, wound care, puncture wound, infection prevention, bathing alternatives, healthcare providers, monitoring complications, persistent pain, changes in sensation, unusual discharge, recovery strategies
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.