Hypertension, or high blood pressure, affects nearly half of adults globally, as reported by the World Health Organization (WHO). It is a leading cause of heart disease, stroke, and kidney failure, and its complications account for a significant proportion of healthcare costs worldwide. For patients with severe or treatment-resistant hypertension, conventional therapies such as medications and lifestyle changes may not suffice. This has spurred interest in advanced bioengineering solutions, particularly artificial organs, as a potential avenue for managing or even reversing the effects of chronic hypertension. This article explores how artificial organs might support patients with severe hypertension, examining the science, current developments, and future possibilities in this innovative field.
You May Also Like: Hypertension and Robotics: A Future of Automated Diagnostics and Treatment
Understanding Severe Hypertension and Its Challenges
What Is Severe Hypertension?
Severe hypertension, often referred to as resistant or refractory hypertension, is characterized by consistently high blood pressure (≥140/90 mmHg) that persists despite the use of three or more antihypertensive medications, including a diuretic. It may be caused by a combination of genetic, environmental, and physiological factors.
Complications of Severe Hypertension
Chronic high blood pressure damages vital organs and systems over time. Key complications include:
- Heart Damage: Left ventricular hypertrophy and increased risk of heart failure.
- Kidney Failure: Reduced renal function due to persistent high pressure in renal arteries.
- Vascular Issues: Atherosclerosis, aneurysms, and arterial stiffening.
- Neurological Effects: Increased risk of stroke and cognitive decline.
For patients who fail to respond to traditional treatments, bioengineering solutions such as artificial organs may offer new hope.

What Are Artificial Organs?
Artificial organs are bioengineered devices designed to replace or support the function of damaged or failing biological organs. These can be mechanical, biological, or hybrid systems and may be implanted, external, or wearable.
Types of Artificial Organs Relevant to Hypertension
Several artificial organs and bioengineering technologies are being explored for their potential to manage hypertension:
- Artificial Kidneys: Designed to enhance or replace kidney function, addressing hypertension caused by chronic kidney disease (CKD).
- Bioengineered Blood Vessels: Used to improve vascular compliance and reduce arterial stiffness, a key contributor to hypertension.
- Heart Support Devices: Such as ventricular assist devices (VADs) and artificial hearts, which help manage hypertension-induced heart failure.
- Neuromodulation Implants: Devices targeting the nervous system to regulate blood pressure.
The Role of Artificial Organs in Hypertension Management
Artificial organs offer targeted solutions for managing hypertension by addressing specific underlying causes. Below are some of the most promising applications:
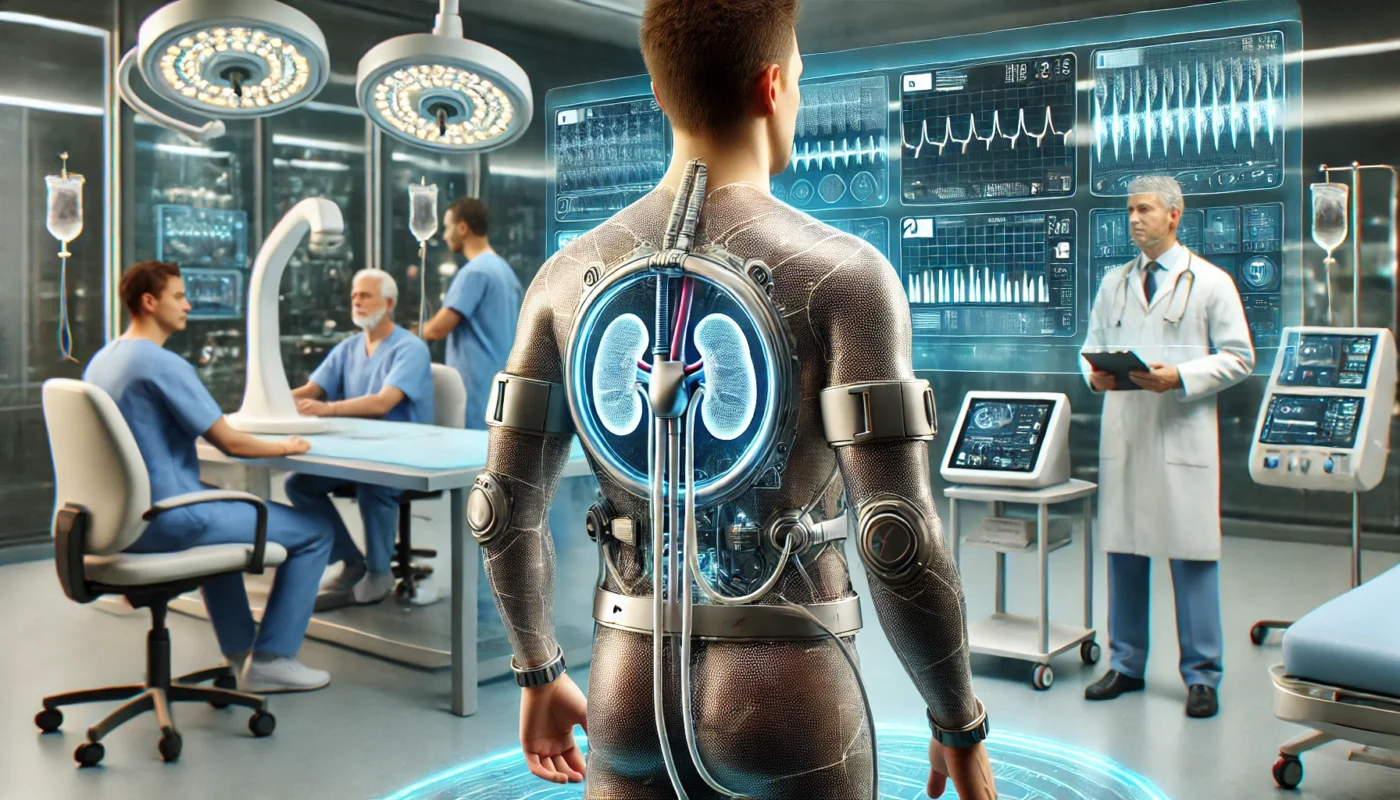
1. Artificial Kidneys for Renal Hypertension
Renal hypertension, caused by impaired kidney function, is one of the most common forms of secondary hypertension. Artificial kidneys, either wearable or implantable, could help by improving waste filtration, regulating fluid balance, and maintaining electrolyte homeostasis.
- Current Developments: The Wearable Artificial Kidney (WAK), a device under clinical trials, provides continuous dialysis to patients with kidney failure. By mimicking the filtration function of healthy kidneys, it can reduce fluid overload and lower blood pressure.
- Potential Impact: Artificial kidneys could significantly reduce the burden of hypertension in patients with chronic kidney disease, offering better control of blood pressure and reducing the need for conventional dialysis.
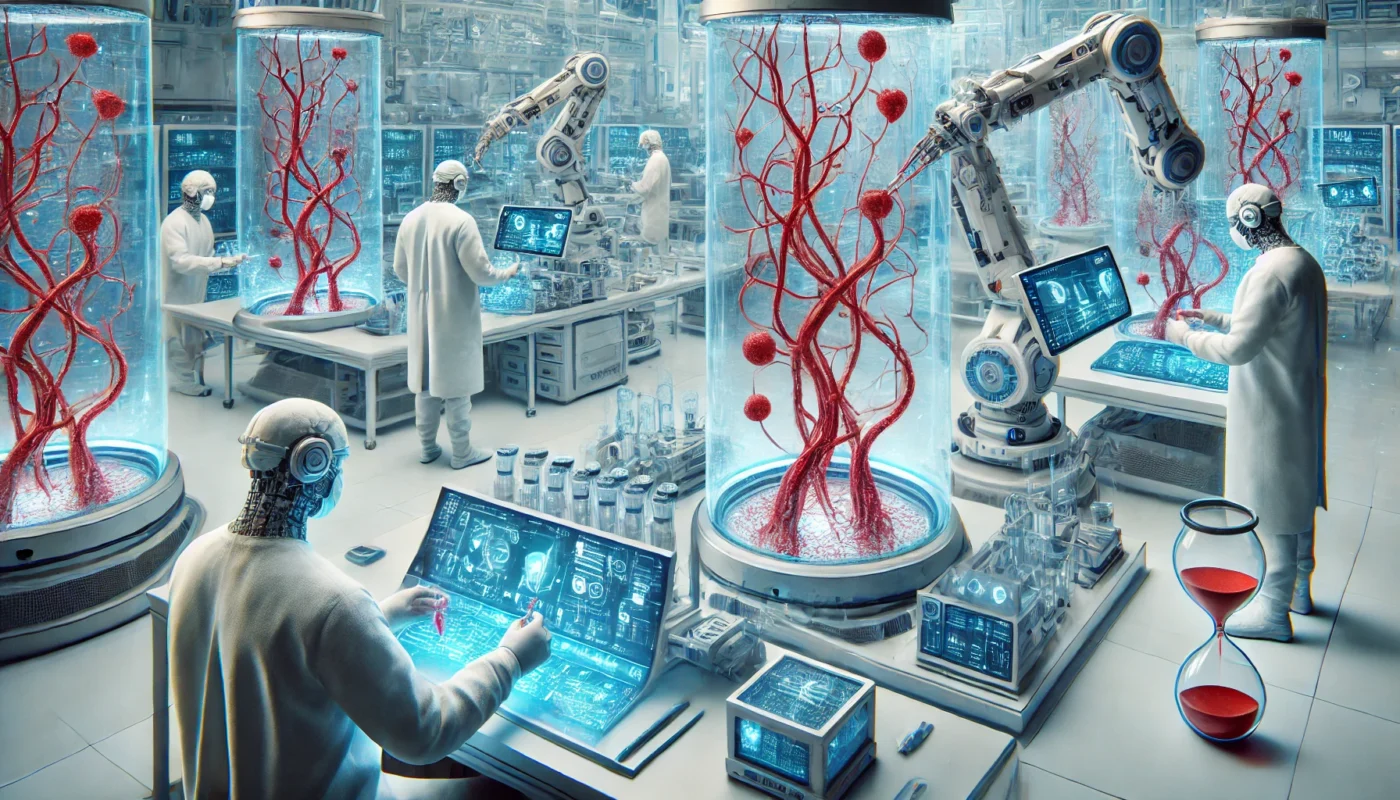
2. Bioengineered Blood Vessels to Reduce Vascular Resistance
Stiffened arteries and reduced vascular compliance are hallmarks of chronic hypertension. Bioengineered blood vessels, made from synthetic or biological materials, aim to restore vascular elasticity and improve blood flow dynamics.
- Science Behind the Technology: These vessels are designed to mimic the biomechanical properties of healthy arteries, reducing systemic vascular resistance and alleviating hypertension.
- Clinical Potential: For patients with severe arterial damage or aneurysms, bioengineered vessels could prevent further complications while addressing the root causes of hypertension.
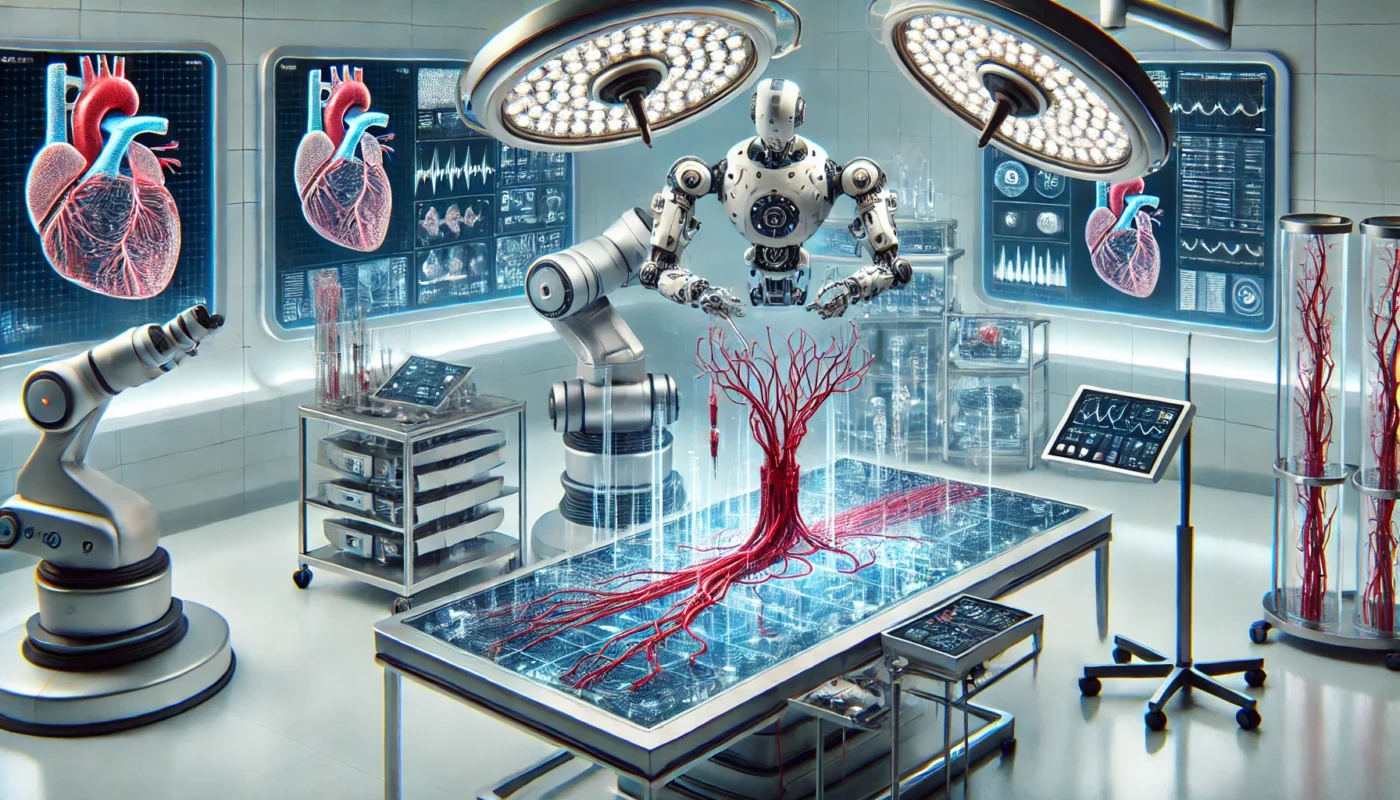
3. Artificial Hearts and Ventricular Assist Devices
Hypertension-induced heart damage can lead to heart failure, requiring advanced cardiac support. Artificial hearts and ventricular assist devices (VADs) are used to support or replace heart function.
- How They Help: By ensuring efficient blood circulation, these devices reduce the workload on the heart, mitigating hypertension’s effects on cardiac function.
- Future Directions: Fully implantable artificial hearts with integrated blood pressure regulation systems are being developed to address the dual challenge of heart failure and hypertension.
4. Neuromodulation Devices for Blood Pressure Control
Neuromodulation implants, such as baroreceptor activation therapy devices, target the nervous system to regulate blood pressure.
- Mechanism of Action: These devices stimulate baroreceptors (pressure sensors in blood vessels) to trigger reflexes that lower blood pressure.
- Clinical Evidence: Studies published in Hypertension (2019) have demonstrated significant reductions in systolic blood pressure with baroreceptor activation therapy in patients with resistant hypertension.
- Limitations: These devices are still undergoing refinement to improve efficacy and minimize side effects.
Challenges and Ethical Considerations in Artificial Organ Use
Challenges
- High Costs: Artificial organ technologies are expensive, limiting accessibility.
- Biocompatibility Issues: Long-term implantation risks include infection, clot formation, and immune rejection.
- Technical Limitations: Devices may require frequent maintenance or replacement.
Ethical Considerations
- Allocation of Resources: With limited availability, determining who receives artificial organs poses ethical dilemmas.
- Informed Consent: Patients must understand the risks and benefits of these experimental technologies.
The Future of Artificial Organs in Hypertension Treatment
As technology advances, artificial organs are becoming more sophisticated, miniaturized, and effective. Below are some anticipated developments:
1. Wearable and Portable Devices
Devices such as wearable kidneys and blood pressure regulators could provide non-invasive solutions for managing hypertension in real-time.
2. Integration with Artificial Intelligence
AI-powered artificial organs could adapt to changes in the body, providing dynamic blood pressure regulation and personalized treatment.
3. Regenerative Medicine
Combining artificial organ technology with stem cells and tissue engineering could lead to hybrid organs that repair and replace damaged tissues while improving blood pressure control.

The Role of Nutritional Supplements in Supporting Artificial Organ Use
While artificial organs address severe hypertension directly, nutritional supplements can play a supportive role in managing blood pressure and maintaining overall health. Below are five supplements that may complement artificial organ therapies:
1. Beetroot Powder
Beetroot enhances nitric oxide levels, improving blood flow and reducing arterial stiffness. Research in Nutrition Journal (2017) showed a 4 mmHg reduction in systolic blood pressure with beetroot supplementation.
2. Magnesium Glycinate
Magnesium relaxes blood vessels and supports electrolyte balance, essential for patients with renal hypertension. A study in Magnesium Research (2016) showed a 5 mmHg reduction in systolic blood pressure with magnesium supplementation.
3. Coenzyme Q10 (CoQ10)
CoQ10 enhances mitochondrial function and reduces oxidative stress, supporting cardiovascular health in patients using artificial hearts or VADs. A clinical trial in Hypertension Research (2007) reported an 11 mmHg reduction in systolic blood pressure with CoQ10 supplementation.
4. Omega-3 Fatty Acids
Omega-3s improve vascular health and reduce inflammation, benefiting patients with bioengineered blood vessels or neuromodulation devices. A meta-analysis in Hypertension (2018) demonstrated a 4 mmHg reduction in systolic blood pressure with omega-3 supplementation.
5. Hibiscus Extract
Hibiscus supports nitric oxide production and improves vascular function, complementing artificial organ therapies. A study in The Journal of Nutrition (2010) found a 6 mmHg reduction in systolic blood pressure with hibiscus supplementation.
Conclusion
Artificial organs represent a groundbreaking frontier in the treatment of severe hypertension. From artificial kidneys and bioengineered blood vessels to neuromodulation implants and heart support devices, these technologies address the underlying causes of hypertension in ways traditional therapies cannot. While challenges remain, advancements in bioengineering, coupled with supportive strategies like nutritional supplementation, promise to revolutionize hypertension management. As the field evolves, artificial organs may not only improve blood pressure control but also enhance the quality of life for patients facing the most severe forms of this condition.
References
- Hypertension. (2019). Baroreceptor activation therapy for resistant hypertension. Hypertension. Retrieved from https://www.ahajournals.org
- Magnesium Research. (2016). Magnesium and its role in blood pressure management. Magnesium Research. Retrieved from https://www.springer.com
- Hypertension Research. (2007). CoQ10 supplementation and blood pressure control. Hypertension Research. Retrieved from https://www.nature.com/hr
- The Journal of Nutrition. (2010). Hibiscus tea and its effects on vascular health. The Journal of Nutrition. Retrieved from https://academic.oup.com
- Nutrition Journal. (2017). The impact of beetroot powder on blood pressure. Nutrition Journal. Retrieved from https://www.biomedcentral.com
Key TERMS for this article:
Hypertension, Artificial Organs, Bioengineering, Resistant Hypertension, Artificial Kidneys, Neuromodulation Devices, Vascular Health
Relevant and useful TAGS for this article:
Hypertension, Artificial Organs, Bioengineering, Kidney Health, Cardiovascular Health, Neuromodulation, Advanced Therapies, Blood Pressure Control, Medical Innovation, Health Technology
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.