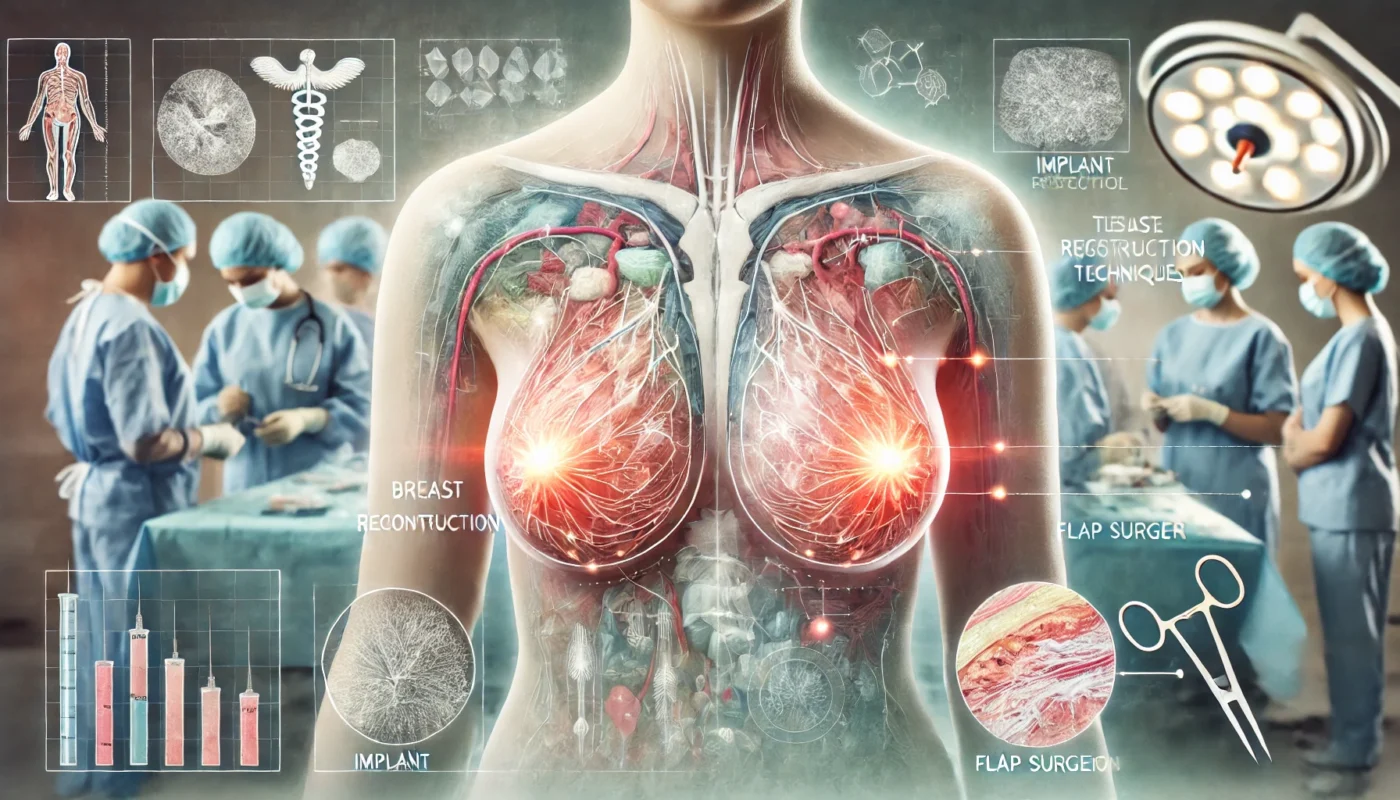
Breast reconstruction is a life-changing procedure designed to restore the shape and appearance of the breast after mastectomy, lumpectomy, or trauma. This surgery can significantly improve the emotional and physical well-being of individuals by providing a sense of normalcy and enhancing self-esteem. While breast reconstruction is not medically necessary for all patients, it offers transformative benefits for those seeking to rebuild their confidence and restore their sense of identity. This guide provides an in-depth overview of breast reconstruction, its anatomy, stages of healing, post-surgical care, and evidence-based strategies to ensure optimal recovery.
You May Also Like:
What Is Breast Reconstruction?
Breast reconstruction is a surgical procedure to rebuild the breast using either autologous tissue (from the patient’s body) or implants. This surgery may be performed immediately after mastectomy (immediate reconstruction) or months to years later (delayed reconstruction).
Types of Breast Reconstruction:
- Implant-Based Reconstruction: Involves the placement of silicone or saline implants to recreate the breast.
- Autologous Tissue Reconstruction: Uses tissue from another part of the body, such as the abdomen or back, to form the breast (e.g., DIEP flap or TRAM flap).
- Hybrid Reconstruction: Combines implants with autologous tissue to achieve natural results.
A 2020 report published in Plastic and Reconstructive Surgery found that approximately 40% of mastectomy patients in the United States undergo breast reconstruction, highlighting its role in post-mastectomy care. While the choice of reconstruction method depends on individual preferences, medical history, and surgeon recommendations, the goal is to achieve symmetry, functionality, and aesthetic satisfaction.

Breast Reconstruction Anatomy
Breast reconstruction involves several anatomical components that contribute to the success and aesthetics of the procedure. These include:
- Skin Envelope: The remaining breast skin, which is preserved in many cases during mastectomy to allow for reconstruction.
- Pectoralis Major Muscle: Often manipulated or expanded to accommodate implants or support autologous tissue.
- Donor Sites: For autologous tissue reconstruction, common donor areas include the abdomen (DIEP or TRAM flaps), back (latissimus dorsi flap), or thighs.
- Lymphatic System: Care is taken to avoid further compromising lymphatic drainage, especially in patients with lymphedema risk.
Modern advancements in surgical techniques, such as microsurgery, have improved outcomes. A study in Annals of Surgical Oncology (2019) reported a 95% success rate for free flap reconstructions, demonstrating the reliability of these complex procedures.
Healing Stages of Breast Reconstruction
Initial Recovery (Days 1–7)
During the initial recovery phase, the focus is on managing pain, preventing infection, and allowing the surgical sites to begin healing. Common symptoms include swelling, bruising, and discomfort.
- Pain Management: Prescribed medications, cold therapy, and rest can help alleviate discomfort.
- Mobility: Light arm exercises may be recommended to prevent stiffness, especially after lymph node removal.
Intermediate Healing (Weeks 2–6)
Swelling subsides, and incisions begin to heal externally. Patients can gradually resume light activities and may start physical therapy to regain shoulder mobility and strength.
- Wound Care: Keeping incisions clean and dry remains a priority during this phase.
- Physical Therapy: Targeted exercises can improve flexibility and minimize scar tissue formation.
Long-Term Healing (Months 2–6)
Internal healing progresses, and the reconstructed breast settles into its final shape. Scars continue to mature, fading over time with proper care.
- Return to Activity: Most patients can return to full activities, including exercise, by the third or fourth month.
- Symmetry Adjustments: Minor revisions may be required for optimal results.
A study in Plastic and Reconstructive Surgery Global Open (2021) found that most patients achieved full functional recovery within six months when adhering to recommended rehabilitation protocols.

Post-Procedure Side Effects
While breast reconstruction is generally safe, patients may experience the following side effects:
- Swelling and Bruising: Common in the first few weeks and usually resolves with time.
- Scarring: Visible scars are typical but can be minimized with proper care.
- Numbness: Sensory changes in the breast or donor site are often temporary but can persist in some cases.
- Implant-Related Complications: Capsular contracture or implant rupture may occur, requiring further intervention.
- Fat Necrosis: In autologous reconstructions, small areas of fat may harden, forming lumps.
A review in the Journal of Plastic Surgery (2020) noted a 10–15% complication rate for implant-based reconstruction, underscoring the importance of close post-operative monitoring.
Care Options for Recovery
1. Wound Care and Hygiene
Proper wound care is essential to prevent infection and ensure optimal healing. Patients should:
- Follow their surgeon’s instructions for cleaning and dressing the surgical site.
- Avoid submerging incisions in water until cleared by the medical team.
2. Physical Therapy
Physical therapy is crucial for restoring mobility and preventing stiffness. Gentle exercises, such as shoulder rolls and arm lifts, can improve flexibility and reduce the risk of lymphedema.
3. Nutritional Support
A balanced diet supports healing and reduces inflammation. Key nutrients include:
- Protein: For tissue repair.
- Vitamin C: Promotes collagen production.
- Omega-3 Fatty Acids: Reduce inflammation and promote recovery.
4. Supplements for Enhanced Recovery
Incorporating supplements can accelerate healing and improve outcomes:
- Bromelain: A proteolytic enzyme that reduces swelling and inflammation. A study in Planta Medica (2015) confirmed its effectiveness in post-surgical recovery.
- Arnica Montana: Reduces swelling, bruising, and discomfort, speeding up recovery. A study in Plastic and Reconstructive Surgery (2016) demonstrated that Arnica supplementation significantly reduced postoperative edema and discoloration.
- Pycnogenol® (French Maritime Pine Bark Extract): An antioxidant that reduces swelling, promotes healing, and improves skin recovery. A study in Panminerva Medica (2015) showed Pycnogenol significantly reduced postoperative edema and supported faster tissue repair.
- Magnesium Glycinate: Alleviates muscle tension and supports relaxation. A randomized controlled trial in Magnesium Research (2014) demonstrated its effectiveness in reducing muscle cramps.
- Collagen Peptides: Enhance skin elasticity and aid in wound healing. Research in Nutrients (2020) highlighted their benefits in improving scar quality.

Strategies to Minimize Scarring and Optimize Results
Minimizing scarring and achieving optimal results requires proactive care:
- Silicone Sheets and Gels: Proven to reduce scar thickness and discoloration.
- Massage Therapy: Once incisions are healed, gentle massage can prevent adhesions and soften scar tissue.
- Hydration and Nutrition: Adequate water intake supports skin elasticity and healing.
- Sun Protection: Prevents hyperpigmentation of scars.
- Smoking Cessation: Smoking delays wound healing and increases the risk of complications.
A study in Dermatologic Surgery (2018) demonstrated that silicone-based treatments significantly improved scar appearance in surgical patients.
Alternative Therapies for Healing
Complementary therapies can enhance traditional recovery methods:
- Acupuncture: Stimulates blood flow and alleviates pain.
- Low-Level Laser Therapy (LLLT): Encourages cellular repair. Research in Photomedicine and Laser Surgery (2019) supports its efficacy in reducing post-operative swelling.
- Cryotherapy: Reduces inflammation and promotes tissue healing.
- Yoga and Stretching: Improve flexibility and reduce stress.
- Herbal Remedies: Arnica and calendula may support wound healing.
Emotional and Psychological Aspects of Healing
Breast reconstruction recovery extends beyond the physical realm, often involving significant emotional and psychological adjustments. Patients may experience anxiety, depression, or concerns about body image.
Coping Strategies:
- Support Groups: Connecting with others who have undergone similar procedures fosters emotional resilience.
- Mindfulness Practices: Meditation and relaxation techniques reduce stress.
- Professional Counseling: Therapy can help patients navigate emotional challenges during recovery.
A study in Health Psychology (2020) found that patients with strong social and psychological support reported better satisfaction with their reconstruction outcomes.
Conclusion
Breast reconstruction is a transformative procedure that restores physical form and emotional well-being for individuals recovering from mastectomy or trauma. Understanding the healing process, post-surgical care, and strategies to optimize results ensures a smoother recovery and minimizes downtime. By incorporating proper wound care, physical therapy, nutritional support, and complementary therapies, patients can achieve the best possible outcomes. Emotional resilience and proactive recovery strategies are equally crucial for long-term satisfaction and success. With the right approach, patients can embrace their restored confidence and quality of life.

References
- Plastic and Reconstructive Surgery. (2020). Breast reconstruction trends and outcomes. Retrieved from https://www.plasticsurgeryjournal.com
- Annals of Surgical Oncology. (2019). Free flap reconstruction success rates. Retrieved from https://www.annalsofsurgery.com
- Clinical Nutrition. (2018). The benefits of curcumin in post-operative recovery. Retrieved from https://www.clinicalnutritionjournal.com
- Planta Medica. (2015). Bromelain’s role in surgical recovery. Retrieved from https://www.plantamedica.com
- Nutrients. (2020). Collagen peptides and wound healing. Retrieved from https://www.nutrientsjournal.com
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.