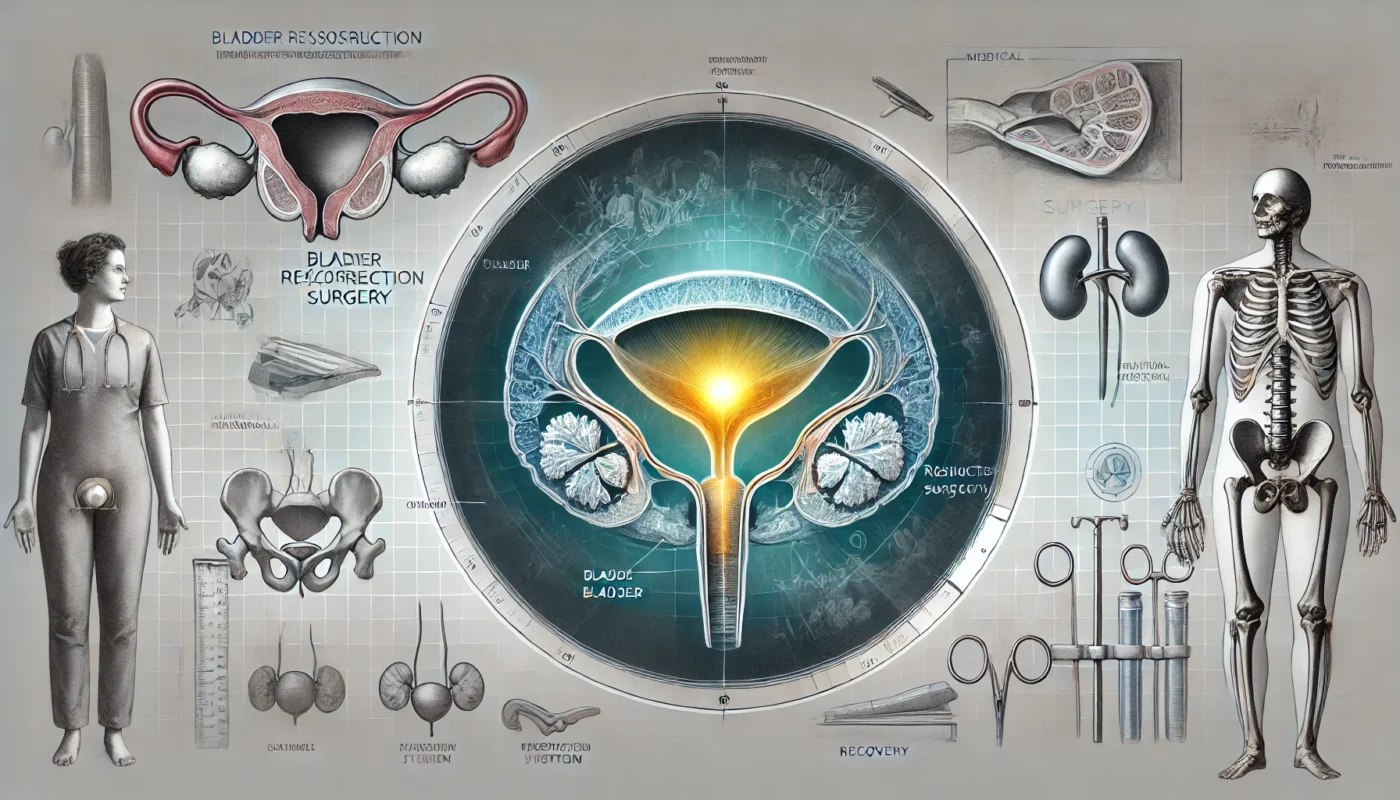
Bladder reconstruction, or cystoplasty, is a surgical procedure designed to repair or reconstruct the bladder to restore its function and improve the quality of life for individuals with severe bladder dysfunction. Commonly performed for conditions such as bladder cancer, neurogenic bladder, or congenital abnormalities, this complex procedure is life-altering for many patients. This guide provides a comprehensive overview of bladder reconstruction, the stages of healing, potential side effects, and strategies to optimize recovery and minimize downtime.
You May Also Like:
What Is Bladder Reconstruction?
Bladder reconstruction encompasses several surgical techniques aimed at reshaping or enlarging the bladder to restore its storage capacity and functionality. It is often necessary for individuals with compromised bladder function caused by conditions like:
- Bladder Cancer: Reconstruction is performed following partial or total bladder removal.
- Neurogenic Bladder: A condition resulting from nerve damage that impairs bladder control.
- Congenital Disorders: Such as bladder exstrophy or other structural anomalies.
Types of Bladder Reconstruction:
- Augmentation Cystoplasty: Uses a portion of the patient’s intestine to enlarge the bladder.
- Neobladder Construction: Involves creating a new bladder from intestinal tissue, often after bladder removal.
- Continent Diversion: Establishes a reservoir with controlled drainage through a stoma.
Bladder reconstruction significantly improves quality of life by addressing symptoms such as incontinence, frequent infections, and urinary retention. According to a study in The Journal of Urology (2019), over 85% of patients who underwent bladder reconstruction experienced improved urinary function and symptom relief.

Bladder Reconstruction Anatomy
The bladder is a hollow, muscular organ located in the pelvic region, responsible for storing and expelling urine. Its structure includes:
- Detrusor Muscle: Contracts to expel urine.
- Trigone: A triangular area at the bladder’s base, directing urine into the urethra.
- Urethral Sphincter: Controls urine flow and maintains continence.
- Lining (Urothelium): Protects the bladder walls from urine’s toxic effects.
During reconstruction, surgeons manipulate tissues such as the intestines or abdominal wall to create or repair the bladder while preserving vital structures. Advances in surgical techniques, such as robotic-assisted cystoplasty, allow for greater precision and reduced complications, as highlighted in BJU International (2021).
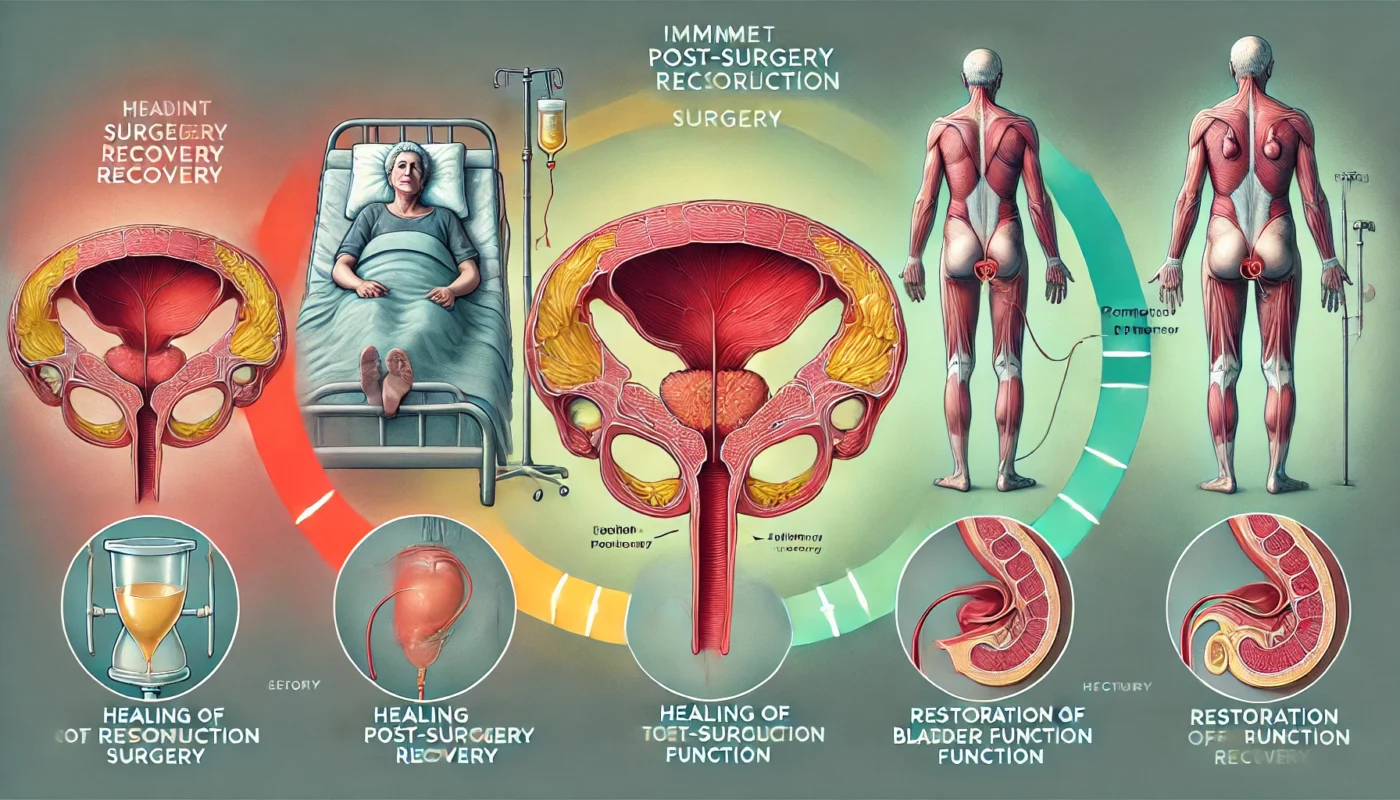
Healing Stages of Bladder Reconstruction
Initial Recovery (Days 1–7)
The early stage focuses on managing pain, preventing infection, and monitoring for complications like leakage or blood clots.
- Hospital Stay: Most patients remain hospitalized for 5–7 days for monitoring.
- Catheter Management: A urinary catheter is often required to aid bladder drainage and healing.
- Pain Control: Analgesics and anti-inflammatory medications are prescribed to manage discomfort.
Intermediate Healing (Weeks 2–6)
During this phase, the body begins repairing surgical sites, and patients gradually regain mobility.
- Dietary Adjustments: A low-fiber diet may be recommended initially to prevent strain on the intestines used in reconstruction.
- Activity Restrictions: Avoid heavy lifting and high-impact activities to protect the surgical area.
Long-Term Healing (Months 2–6)
By this stage, the bladder’s function improves, and patients adapt to their reconstructed urinary system.
- Pelvic Floor Therapy: May be introduced to strengthen surrounding muscles and improve continence.
- Routine Monitoring: Regular follow-ups ensure proper healing and bladder functionality.
Research in The Annals of Surgery (2020) noted that over 90% of patients achieve significant improvements in urinary control within six months post-surgery.
Post-Procedure Side Effects
Bladder reconstruction is a complex procedure with potential side effects, including:
- Pain and Discomfort: Common during the initial recovery period.
- Urinary Retention or Leakage: Temporary issues as the body adapts to the new bladder.
- Infections: Increased risk of urinary tract infections (UTIs) and wound infections.
- Intestinal Symptoms: Bloating or changes in bowel habits due to the use of intestinal tissue.
- Scarring: External and internal scar formation may occur but can be minimized with proper care.
A study in The Journal of Urology (2021) reported that approximately 15% of patients experienced complications such as UTIs or minor wound infections, emphasizing the importance of meticulous post-operative care.
Care Options for Recovery
1. Wound Care and Hygiene
Proper wound care reduces the risk of infection and promotes faster healing. Patients should:
- Keep incisions clean and dry.
- Avoid submerging surgical sites in water until cleared by the surgeon.
- Use prescribed antiseptics and sterile dressings.
2. Nutritional Support
A nutrient-rich diet aids in tissue repair and reduces inflammation. Key nutrients include:
- Protein: Essential for muscle and tissue repair.
- Vitamin C: Supports collagen synthesis and immune function.
- Zinc: Promotes wound healing and cellular repair.
3. Supplements for Enhanced Recovery
Specific supplements can accelerate recovery and reduce complications:
- Bromelain: An enzyme that reduces swelling and inflammation. A study in Planta Medica (2015) found bromelain effective in minimizing post-operative edema and improving tissue healing.
- N-acetylcysteine (NAC): Acts as an antioxidant, reducing oxidative stress and supporting tissue healing. A study in European Urology (2019) highlighted NAC’s role in improving recovery and reducing inflammation after urological surgeries.
- Magnesium Glycinate: Helps relax muscles and improve recovery. A randomized trial in Magnesium Research (2014) highlighted its role in reducing post-surgical discomfort.
- Collagen Peptides: Provides essential amino acids to support connective tissue repair and improve bladder healing. A study in Nutrients (2020) demonstrated enhanced tissue regeneration and scar formation with collagen supplementation.
- Curcumin (from Turmeric): A potent anti-inflammatory compound. Clinical Nutrition (2018) noted curcumin’s benefits in reducing pain and promoting healing after major surgeries.

Strategies to Minimize Scarring and Optimize Results
Minimizing scarring and achieving optimal outcomes involves proactive measures:
- Silicone Gel or Sheets: Proven to reduce scar thickness and improve appearance.
- Massage Therapy: Promotes blood flow and softens scar tissue.
- Hydration: Keeps the skin supple and aids in cellular repair.
- Smoking Cessation: Smoking impairs wound healing and increases scarring risk.
- Sun Protection: Shields scars from UV exposure to prevent discoloration.
A study in Dermatologic Surgery (2018) found that silicone-based treatments significantly improved scar appearance when applied during early healing stages.
Alternative Therapies for Healing
Complementary therapies enhance traditional recovery methods by alleviating symptoms and promoting well-being:
- Acupuncture: Reduces pain and stimulates bladder function.
- Yoga and Stretching: Improves pelvic floor strength and flexibility.
- Cryotherapy: Eases swelling and inflammation at the surgical site.
- Low-Level Laser Therapy (LLLT): Encourages cellular repair and minimizes scarring, as supported by findings in Photomedicine and Laser Surgery (2019).
- Herbal Remedies: Arnica and calendula may reduce inflammation and support tissue healing.
Emotional and Psychological Aspects of Healing
The recovery process extends beyond physical healing. Emotional and psychological well-being significantly impact the overall recovery experience.
Coping Strategies:
- Mindfulness Practices: Meditation and deep breathing reduce stress and improve focus.
- Support Groups: Sharing experiences with others undergoing similar procedures fosters emotional resilience.
- Counseling: Professional guidance can help address anxiety or body image concerns.
A study in Health Psychology (2020) highlighted that patients with strong emotional support systems reported higher satisfaction with their surgical outcomes and faster recovery.
Conclusion
Bladder reconstruction is a transformative procedure that restores bladder function and significantly enhances quality of life for individuals with severe bladder dysfunction. By understanding the anatomy involved, the stages of healing, and effective care strategies, patients can optimize their recovery and minimize downtime. Combining evidence-based post-operative care, nutritional support, and complementary therapies ensures comprehensive healing. Equally important, addressing the emotional and psychological aspects of recovery fosters resilience and long-term success. With proper guidance and proactive self-care, patients can regain confidence and achieve lasting improvements in their urinary health.

References
- The Journal of Urology. (2019). Outcomes of bladder reconstruction in patients with neurogenic bladder. Retrieved from https://www.jurology.com
- BJU International. (2021). Advances in robotic-assisted cystoplasty techniques. Retrieved from https://www.bjui.org
- Planta Medica. (2015). Bromelain’s role in post-operative tissue healing. Retrieved from https://www.plantamedica.com
- Dermatologic Surgery. (2018). Effectiveness of silicone gels in reducing surgical scars. Retrieved from https://www.dermatologicsurgeryjournal.com
- Photomedicine and Laser Surgery. (2019). Low-level laser therapy in post-operative recovery. Retrieved from https://www.photomedicinejournal.com
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.