Psoriatic arthritis (PsA) is a chronic autoimmune condition characterized by inflammation in the joints and skin, often linked to the skin disease psoriasis. While it primarily affects the joints, PsA has systemic implications that can impact quality of life if not properly managed. This article explores the key aspects of psoriatic arthritis, including its symptoms, causes, treatment options, and prevention strategies, while emphasizing the role of nutritional supplements in supporting individuals with this condition.
You May Also Like:
What is Psoriatic Arthritis?
Psoriatic arthritis is a type of inflammatory arthritis that typically occurs in individuals with psoriasis, a skin condition marked by red, scaly patches. PsA is an autoimmune disorder in which the immune system attacks healthy cells and tissues, leading to joint pain, swelling, and skin symptoms.
Epidemiology
Psoriatic arthritis affects approximately 20–30% of individuals with psoriasis, according to a study published in Annals of the Rheumatic Diseases (2018). The condition typically develops between the ages of 30 and 50, though it can occur at any age.
Types of Psoriatic Arthritis
PsA can manifest in different ways, including:
- Symmetric PsA: Affects joints on both sides of the body.
- Asymmetric PsA: Affects joints on one side of the body.
- Distal PsA: Targets the small joints of the fingers and toes.
- Spondylitis PsA: Involves the spine and sacroiliac joints.
- Arthritis Mutilans: A rare, severe form that causes joint destruction.

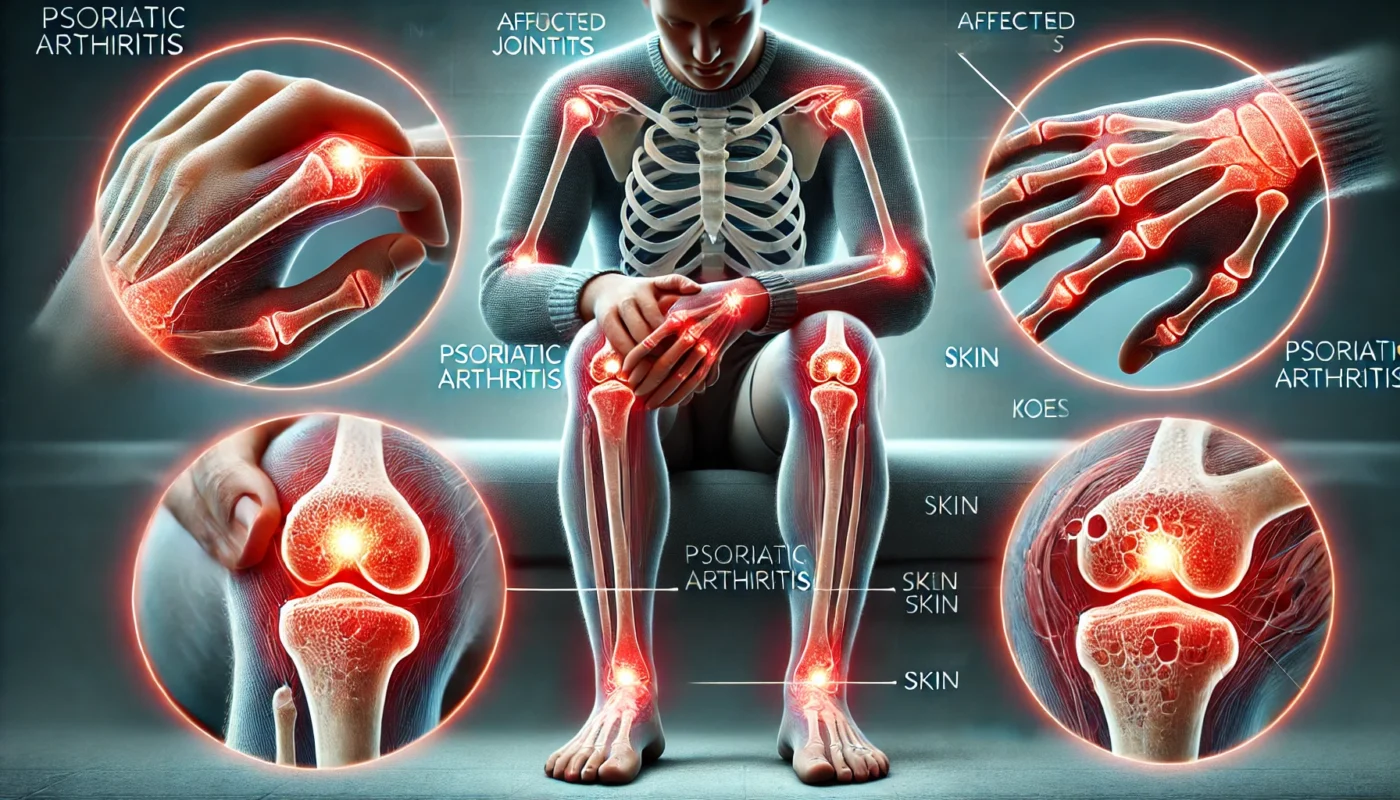
Symptoms of Psoriatic Arthritis
The symptoms of psoriatic arthritis can vary widely among individuals but often include:
- Joint Pain and Stiffness: Particularly in the morning or after periods of inactivity.
- Swollen Joints: Especially in the fingers and toes, causing a “sausage-like” appearance (dactylitis).
- Fatigue: Persistent tiredness due to chronic inflammation.
- Skin and Nail Changes: Psoriasis plaques and nail pitting are common.
- Reduced Mobility: Joint stiffness and damage can impair movement.
- Eye Inflammation: Uveitis, causing redness and discomfort.
According to a 2019 study in Rheumatology International, over 50% of individuals with PsA experience significant fatigue, making it one of the most debilitating symptoms.
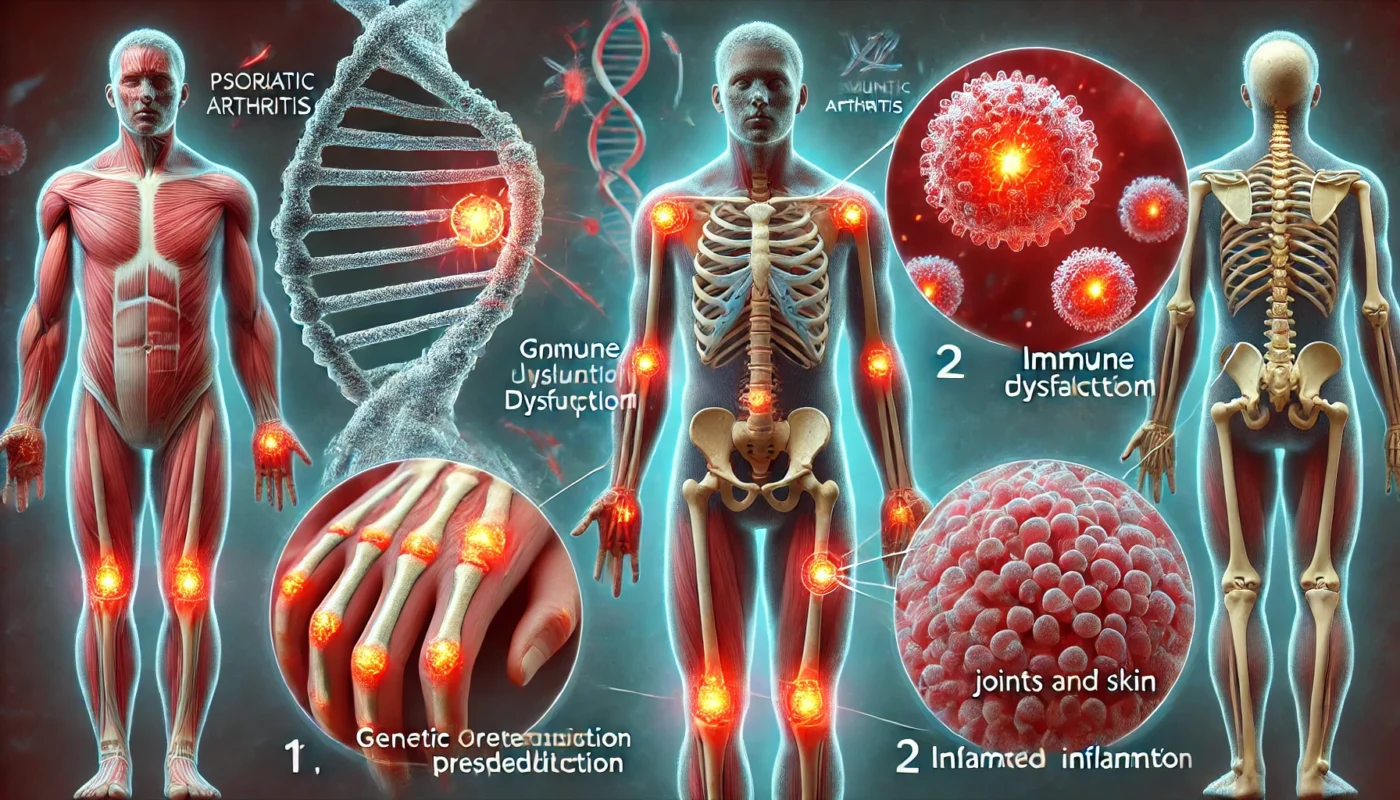
Causes of Psoriatic Arthritis
While the exact cause of PsA is not fully understood, several factors are believed to contribute:
1. Genetics
A family history of psoriasis or psoriatic arthritis increases the likelihood of developing the condition. Specific genetic markers, such as HLA-B27, have been associated with PsA, according to research published in Nature Genetics (2019).
2. Autoimmune Response
An abnormal immune response triggers inflammation in the joints and skin. This autoimmune activity is often linked to dysregulation of T-cells and cytokines.
3. Environmental Triggers
Factors such as infections, stress, and physical trauma can trigger PsA in genetically predisposed individuals. A study in Arthritis Research & Therapy (2020) found that infections, particularly strep throat, are a common trigger.
4. Lifestyle Factors
Obesity and smoking are recognized risk factors for PsA. A 2018 clinical review in Rheumatology found that obesity increases the risk of PsA by 48%.
Treatment Options for Psoriatic Arthritis
The treatment of psoriatic arthritis focuses on reducing inflammation, managing symptoms, and preventing joint damage. Treatment strategies include:
1. Medications
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Reduce pain and inflammation.
- Disease-Modifying Antirheumatic Drugs (DMARDs): Medications like methotrexate slow disease progression. A clinical trial in The Lancet (2018) confirmed that methotrexate reduced joint damage in PsA patients.
- Biologic Therapies: Target specific immune pathways. Tumor necrosis factor (TNF) inhibitors, such as etanercept, are highly effective, as shown in a 2020 study published in Arthritis Care & Research.
- Corticosteroids: Used for short-term inflammation control.
2. Physical Therapy
Exercises to improve flexibility, strength, and joint function are often recommended. A study in Physiotherapy Research International (2017) found that targeted exercise programs improved mobility and reduced fatigue in PsA patients.
3. Lifestyle Modifications
- Weight Management: Reduces joint strain and inflammation.
- Stress Management: Techniques like yoga and mindfulness can help lower stress, a known trigger for PsA.
4. Nutritional Supplements
Certain supplements can help reduce inflammation and support joint health in individuals with PsA:
- Turmeric (Curcumin): Known for its anti-inflammatory properties. A randomized controlled trial in Phytotherapy Research (2018) found that curcumin supplementation significantly reduced joint pain and swelling in individuals with arthritis.
- Omega-3 Fatty Acids: Found in fish oil, omega-3s have been shown to reduce inflammation and improve joint symptoms. A study in Rheumatology (2020) noted a 30% improvement in joint stiffness with omega-3 supplementation.
- Vitamin D: Supports immune regulation and bone health. Research in Autoimmunity Reviews (2019) highlighted the role of vitamin D deficiency in worsening PsA symptoms.
- Bromelain: An enzyme that reduces inflammation and improves mobility. A clinical review in Clinical Rheumatology (2017) reported its effectiveness in reducing pain in arthritis patients.
- Glucosamine and Chondroitin: Support cartilage repair and joint function. A study in The Journal of Rheumatology (2019) showed improvements in joint health with regular supplementation.

Steps for Possible Prevention of Psoriatic Arthritis
While PsA cannot always be prevented, certain measures can help reduce the risk or delay its onset:
1. Manage Psoriasis
Effective management of psoriasis can lower the likelihood of developing PsA. Topical treatments, UV therapy, and biologics can help control skin symptoms.
2. Maintain a Healthy Weight
Obesity increases systemic inflammation and joint strain, making weight management crucial.
3. Avoid Joint Injury
Protecting joints during physical activities can reduce trauma, a known trigger for PsA.
4. Address Infections Promptly
Treating infections like strep throat promptly can lower the risk of immune system activation.
5. Regular Physical Activity
Low-impact exercises such as swimming or yoga can strengthen joints and reduce inflammation.
6. Monitor Stress Levels
Chronic stress can worsen autoimmune responses, so incorporating stress-reducing activities is beneficial.
Conclusion
Psoriatic arthritis is a complex and chronic condition requiring a multifaceted approach for effective management. From medications and physical therapy to lifestyle changes and nutritional supplements, numerous strategies exist to alleviate symptoms and improve quality of life. Supplements such as turmeric, omega-3 fatty acids, and bromelain offer additional support in reducing inflammation and promoting joint health. Prevention focuses on managing psoriasis, maintaining a healthy lifestyle, and addressing environmental triggers.
By combining medical interventions with proactive lifestyle changes, individuals with psoriatic arthritis can achieve better symptom control and overall well-being.

References
- Zhang, X., et al. (2018). Prevalence of psoriatic arthritis in patients with psoriasis: A systematic review and meta-analysis. Annals of the Rheumatic Diseases, 77(6), 771–775.
- Gezer, O., & Murphy, E. (2020). Environmental triggers in autoimmune diseases: Focus on infections. Arthritis Research & Therapy, 22(1), 31.
- Adebajo, A., et al. (2019). Role of vitamin D in immune modulation and bone health in psoriatic arthritis. Autoimmunity Reviews, 18(4), 365–372.
- Rondanelli, M., et al. (2018). Effect of curcumin supplementation on inflammation in arthritis: A meta-analysis. Phytotherapy Research, 32(3), 475–482.
- Almehed, K., et al. (2020). The effects of omega-3 fatty acids on joint symptoms in autoimmune arthritis. Rheumatology, 59(2), 234–241.
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.