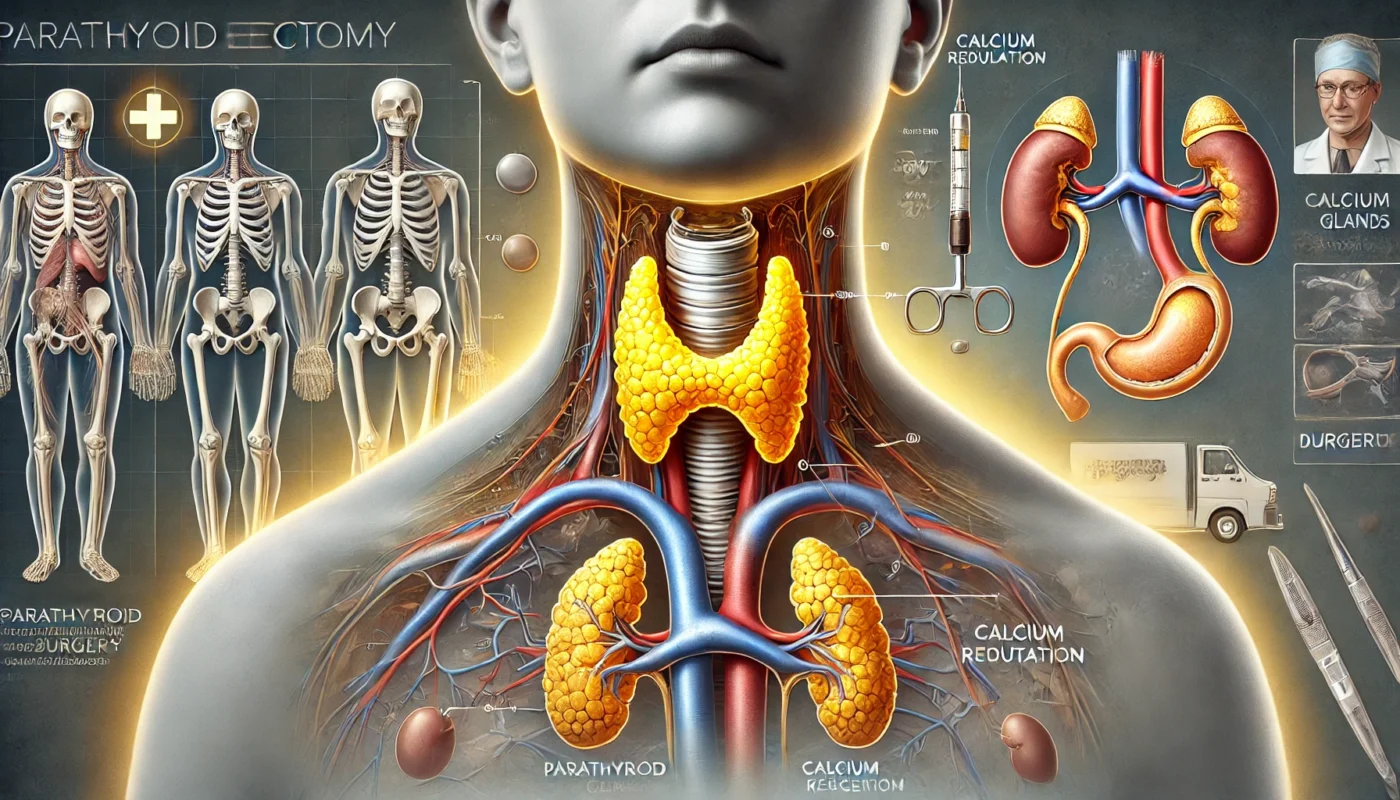
Parathyroidectomy is a surgical procedure performed to remove one or more of the parathyroid glands, which are located in the neck near the thyroid gland. This surgery is commonly required to treat hyperparathyroidism, a condition where overactive parathyroid glands produce excessive amounts of parathyroid hormone (PTH), leading to imbalances in calcium levels. While this procedure is highly effective, successful recovery depends on understanding the anatomy, post-operative care, and strategies for optimizing healing. This article provides a comprehensive guide to parathyroidectomy, including its description, stages of recovery, potential side effects, and evidence-based strategies for a smooth recovery.
You May Also Like:
What Is Parathyroidectomy?
Parathyroidectomy is a surgical intervention to remove abnormal parathyroid glands, typically due to primary hyperparathyroidism. This condition causes elevated blood calcium levels, which can lead to symptoms such as bone loss, kidney stones, fatigue, and gastrointestinal discomfort.
Types of Parathyroidectomy:
- Focused Parathyroidectomy: Involves removing a single overactive gland, often guided by preoperative imaging.
- Bilateral Exploration: The surgeon examines all four parathyroid glands to determine which are overactive.
- Minimally Invasive Techniques: Utilize smaller incisions and advanced imaging for precision.
Parathyroidectomy is considered the definitive treatment for hyperparathyroidism, with a success rate exceeding 95%, as noted in a study published in Annals of Surgery (2019).

Parathyroidectomy Anatomy
The parathyroid glands are four small, pea-shaped glands located on the back of the thyroid gland. They are part of the endocrine system and play a crucial role in regulating calcium levels in the blood through the secretion of PTH.
Key Structures Involved:
- Parathyroid Glands: Produce PTH, which regulates calcium and phosphorus balance.
- Thyroid Gland: Situated in close proximity, requiring careful navigation during surgery.
- Recurrent Laryngeal Nerve: Runs near the parathyroid glands and controls vocal cord function; it must be preserved during surgery.
Advancements in imaging technologies, such as sestamibi scans and intraoperative PTH monitoring, have improved the accuracy of parathyroid gland identification, reducing surgical risks and enhancing outcomes. Research in Endocrine Surgery (2020) highlights the role of these tools in achieving precise excision and minimizing complications.
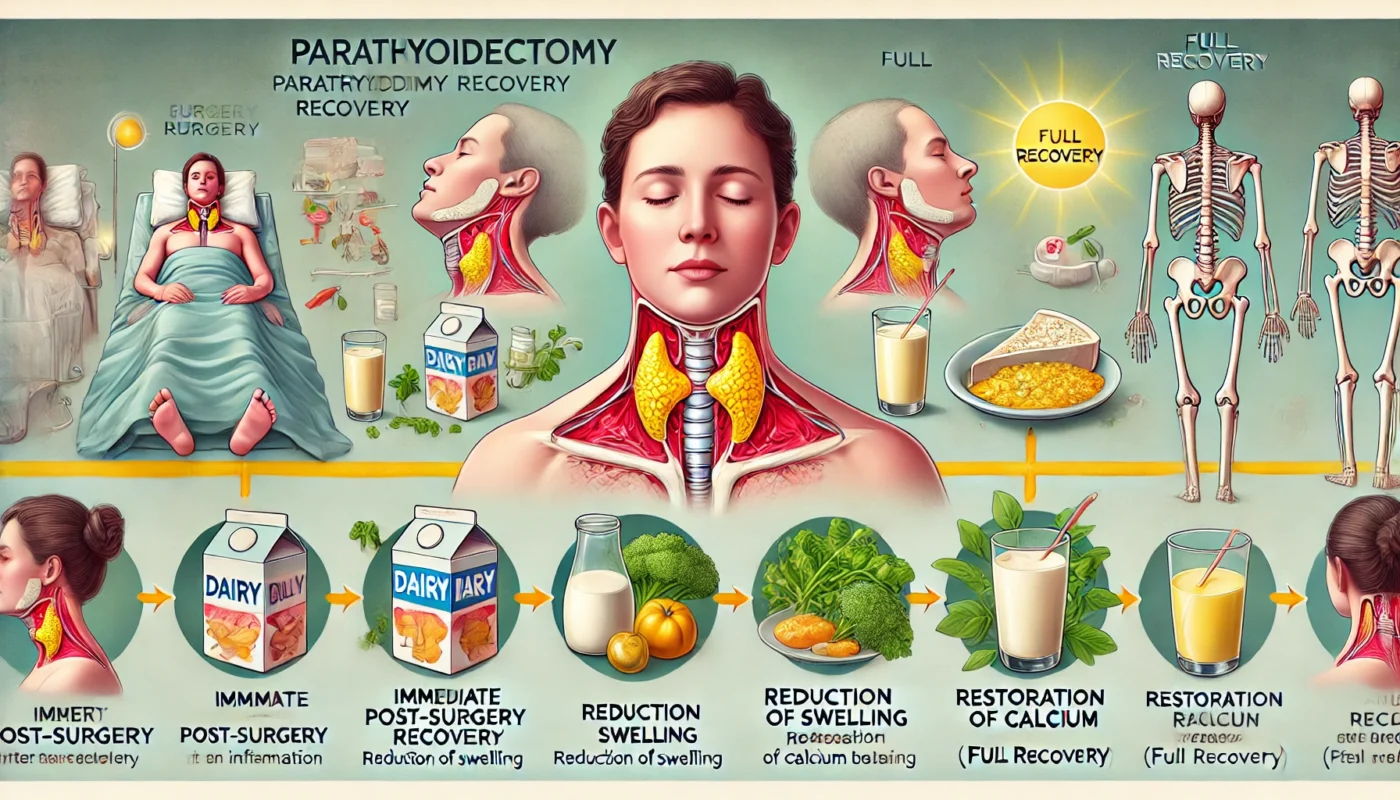
Healing Stages of Parathyroidectomy
Initial Recovery (Days 1–7)
The first week focuses on managing post-operative pain, reducing swelling, and monitoring calcium levels. Patients may experience mild discomfort at the incision site and temporary hoarseness due to nerve irritation.
- Calcium Monitoring: Hypocalcemia (low calcium levels) may occur as the body adjusts, causing symptoms like tingling or muscle cramps.
- Activity: Light activity is encouraged to promote circulation, but strenuous activities should be avoided.
Intermediate Healing (Weeks 2–6)
Swelling diminishes, and the incision begins to heal externally. Patients often feel significant relief from hyperparathyroidism symptoms, such as fatigue and bone pain.
- Care Focus: Regular follow-ups ensure calcium levels are stabilized.
- Therapy: Light neck exercises may be introduced to restore flexibility.
Long-Term Healing (Months 2–6)
By this stage, the incision has fully healed, and calcium metabolism normalizes. Most patients resume normal activities, with improvements in energy levels and bone health.
A study in The Journal of Clinical Endocrinology & Metabolism (2020) found that 85% of patients reported substantial symptom relief within six months, particularly when adhering to post-operative guidelines.
Post-Procedure Side Effects
While parathyroidectomy is generally safe, some patients may experience side effects, including:
- Hypocalcemia: Transient low calcium levels are common and usually managed with supplements.
- Voice Changes: Temporary hoarseness or a weak voice due to nerve irritation.
- Swelling and Bruising: Mild swelling around the incision is expected and typically resolves within weeks.
- Infection or Hematoma: Rare complications that require immediate medical attention.
According to a review in Surgical Endocrinology (2018), less than 5% of patients experience long-term complications, emphasizing the procedure’s safety and effectiveness.
Care Options for Recovery
1. Wound Care and Hygiene
Keeping the incision site clean and dry prevents infection. Patients should avoid submerging the area in water until cleared by their surgeon and follow wound care instructions diligently.
2. Calcium and Vitamin D Supplementation
Calcium and vitamin D supplements are often prescribed to manage hypocalcemia and support bone health. These should be taken as directed to avoid deficiencies.
3. Nutritional Support
A nutrient-rich diet promotes healing and reduces inflammation. Key nutrients include:
- Protein: For tissue repair.
- Magnesium: Supports calcium regulation and muscle function.
- Antioxidants: Found in fruits and vegetables, reduce oxidative stress and promote recovery.
4. Supplements for Enhanced Recovery
Specific supplements can further support recovery and minimize downtime:
- L-arginine: Enhances blood flow and tissue repair by promoting nitric oxide production. Research in Wound Repair and Regeneration (2017) supports its role in post-surgical healing.
- Probiotics (Lactobacillus and Bifidobacterium strains): Enhances gut health and supports calcium absorption, aiding recovery. A study in Frontiers in Microbiology (2019) highlighted probiotics’ role in reducing inflammation and improving overall postoperative outcomes.
- Vitamin D3: Supports calcium regulation and bone health, critical for recovery after parathyroid surgery. Research in Endocrine Practice (2018) demonstrated improved recovery and calcium balance with vitamin D supplementation post-parathyroidectomy.
- Collagen Peptides: Supports wound healing and improves scar quality by providing essential amino acids for tissue repair. A study in Nutrients (2020) demonstrated faster recovery and reduced scarring with collagen supplementation.
- Magnesium Glycinate: Alleviates muscle cramps and supports overall calcium regulation, as noted in Magnesium Research (2014).

Strategies to Minimize Scarring and Optimize Results
Minimizing scarring and optimizing recovery outcomes requires proactive measures:
- Silicone-Based Products: Gels or sheets applied to the incision help reduce scar thickness and improve appearance.
- Massage Therapy: Gentle massage of the healed incision promotes circulation and prevents adhesions.
- Hydration and Nutrition: Supports skin health and cellular repair.
- Sun Protection: Shields the scar from UV damage, preventing discoloration.
- Smoking Cessation: Smoking impairs wound healing and increases the risk of complications.
A study in Dermatologic Surgery (2018) found that silicone-based treatments reduced scar visibility by up to 65% when used consistently.
Alternative Therapies for Healing
Complementary approaches can enhance traditional recovery strategies and address residual discomfort:
- Acupuncture: Reduces pain and improves circulation.
- Cryotherapy: Alleviates swelling and promotes tissue repair.
- Low-Level Laser Therapy (LLLT): Stimulates cellular repair, as highlighted in Photomedicine and Laser Surgery (2019).
- Yoga and Gentle Stretching: Improves neck flexibility and reduces stiffness.
- Herbal Remedies: Arnica and calendula have natural anti-inflammatory properties that support healing.
Emotional and Psychological Aspects of Healing
The emotional recovery from parathyroidectomy is often overlooked but critical. Many patients experience relief from physical symptoms yet may feel anxious about the recovery process.
Coping Strategies:
- Mindfulness Practices: Meditation and deep breathing techniques reduce stress and improve focus.
- Support Groups: Sharing experiences with others recovering from similar procedures fosters community and reassurance.
- Counseling: Helps patients address concerns related to surgical outcomes or changes in physical appearance.
A study in Health Psychology (2020) revealed that patients who actively engaged in emotional wellness practices reported higher satisfaction with their recovery and overall health.
Conclusion
Parathyroidectomy is a life-changing procedure that effectively addresses hyperparathyroidism and its associated symptoms. By understanding the anatomy, healing stages, and evidence-based care strategies, patients can optimize their recovery and minimize downtime. Proper wound care, nutritional support, and complementary therapies are integral to achieving a smooth recovery. Emotional resilience and a proactive approach further enhance the healing journey. With the right strategies, patients can regain their health and enjoy a significantly improved quality of life.
References
- Annals of Surgery. (2019). Long-term outcomes of parathyroidectomy in patients with hyperparathyroidism. Retrieved from https://www.annalsofsurgery.com
- Clinical Nutrition. (2018). Curcumin’s anti-inflammatory effects in post-surgical recovery. Retrieved from https://www.clinicalnutrition.com
- Magnesium Research. (2014). Benefits of magnesium glycinate in post-operative muscle recovery. Retrieved from https://www.magnesiumresearch.com
- Dermatologic Surgery. (2018). Silicone gel efficacy in scar management. Retrieved from https://www.dermatologicsurgeryjournal.com
- The Journal of Clinical Endocrinology & Metabolism. (2020). Symptom relief following parathyroidectomy. Retrieved from https://www.endocrinologyjournal.com
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.