Inflammation is the body’s natural response to harmful stimuli, such as pathogens, damaged cells, or irritants. It is a complex biological response that involves the immune system, blood vessels, and various molecular mediators. The ultimate goal of inflammation is to eliminate the initial cause of cell injury, clear out necrotic cells and tissues, and initiate tissue repair.
You may also like: Key Factors in Proliferative Wound Healing
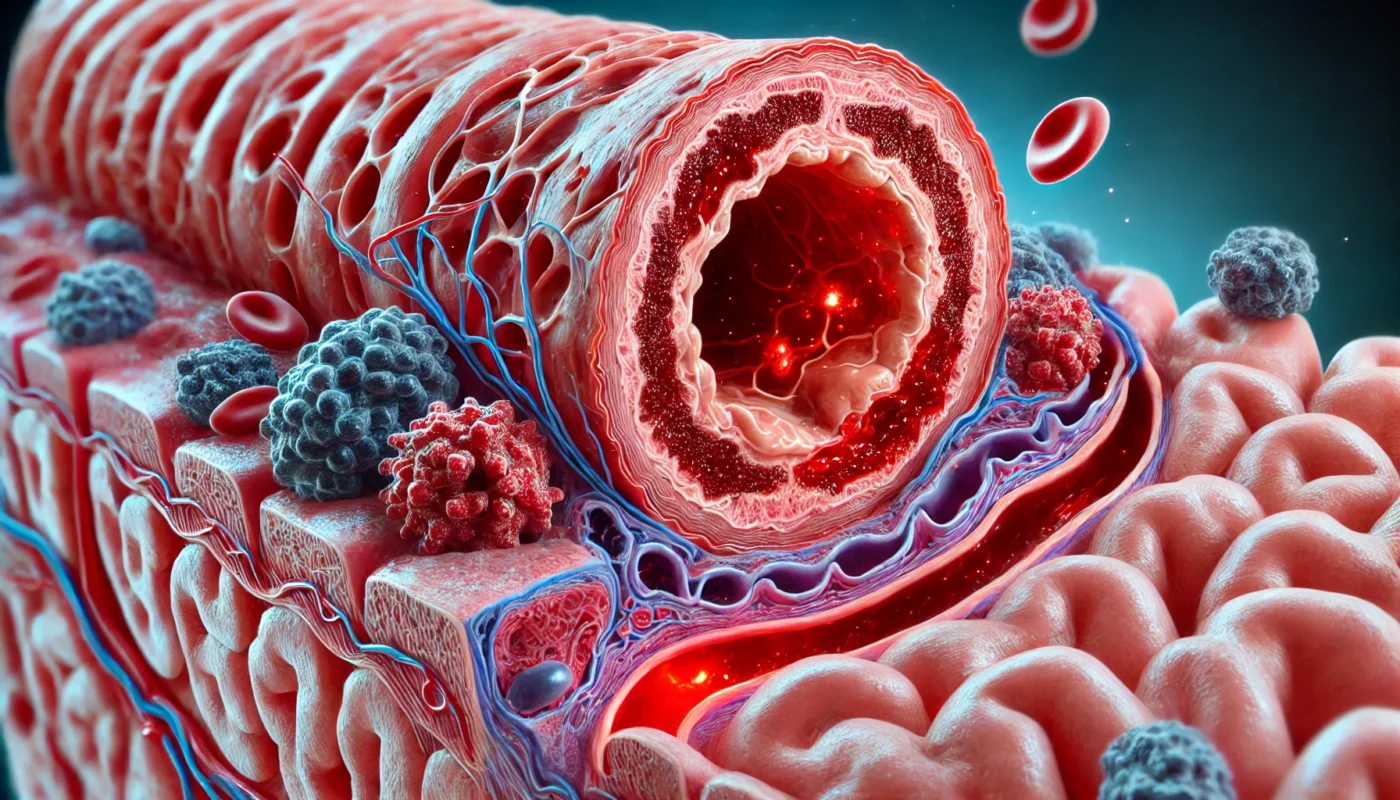
The Biological Mechanism
The inflammatory response is initiated when the body’s immune system recognizes harmful agents or cell damage. This recognition triggers a cascade of events involving various cells, such as white blood cells, and signaling molecules. These components work together to isolate the affected area, preventing the spread of damage.
The process is tightly regulated, with multiple checks and balances to ensure that inflammation occurs only when necessary and is limited in scope. Key players include cytokines, which are signaling proteins, and chemokines, which guide immune cells to the site of injury.
Importance of Inflammation
Inflammation is not just about defense; it is also about repair. By clearing out damaged cells and pathogens, it paves the way for tissue regeneration. This dual role makes it essential for maintaining health and preventing infections from spreading.
However, inflammation must be tightly controlled. If the process becomes excessive or prolonged, it can lead to tissue damage and contribute to various diseases. This underscores the importance of understanding how inflammation works to harness its benefits while minimizing risks.
Factors Influencing Inflammation
Several factors influence the inflammatory response, including genetic predisposition, environmental exposures, and lifestyle choices. For example, some individuals may have a genetic tendency to produce higher levels of inflammatory mediators, making them more prone to inflammation-related conditions.
Environmental factors such as pollution, smoking, and exposure to toxins can also trigger inflammation. Lifestyle choices, including diet, physical activity, and stress levels, play a significant role in either exacerbating or mitigating inflammation.
Acute vs. Chronic Inflammation
Before diving into the inflammatory response phases, it’s essential to distinguish between acute and chronic inflammation. Acute inflammation is the body’s immediate response to injury or infection, characterized by redness, heat, swelling, pain, and loss of function. It is typically short-lived, lasting a few days to a couple of weeks.
Characteristics of Acute Inflammation
Acute inflammation serves as the body’s first line of defense against injury or infection. The hallmark signs—redness, heat, swelling, pain, and loss of function—are due to increased blood flow and immune activity. This phase is crucial for isolating the threat and initiating the healing process.
During acute inflammation, the body increases the production of protective proteins and immune cells. These components work to neutralize pathogens and begin repairing damaged tissues. The process is generally self-limiting, with the body naturally resolving the inflammation once the threat is eliminated.
Transition to Chronic Inflammation
In some cases, acute inflammation fails to resolve, leading to chronic inflammation. This transition can occur when the initial cause of inflammation is not fully addressed, resulting in a persistent immune response. Factors such as ongoing infections, autoimmune reactions, or repeated exposure to irritants can contribute to this shift.
Chronic inflammation is characterized by a different set of immune cells, which can cause tissue damage if the process continues unchecked. The body’s repair mechanisms are activated, but they may not fully restore normal tissue function, leading to fibrosis or scarring.
Health Implications of Chronic Inflammation
Chronic inflammation is associated with a wide range of health issues, from arthritis and diabetes to cardiovascular diseases and cancer. It creates a state of ongoing tissue damage and repair, which can disrupt normal bodily functions. Understanding how to manage chronic inflammation is vital for preventing these associated diseases.
Lifestyle factors, such as diet and stress, play a significant role in chronic inflammation. Addressing these factors through a holistic approach can help reduce chronic inflammation and its health risks. This includes dietary changes, regular exercise, and stress management techniques.
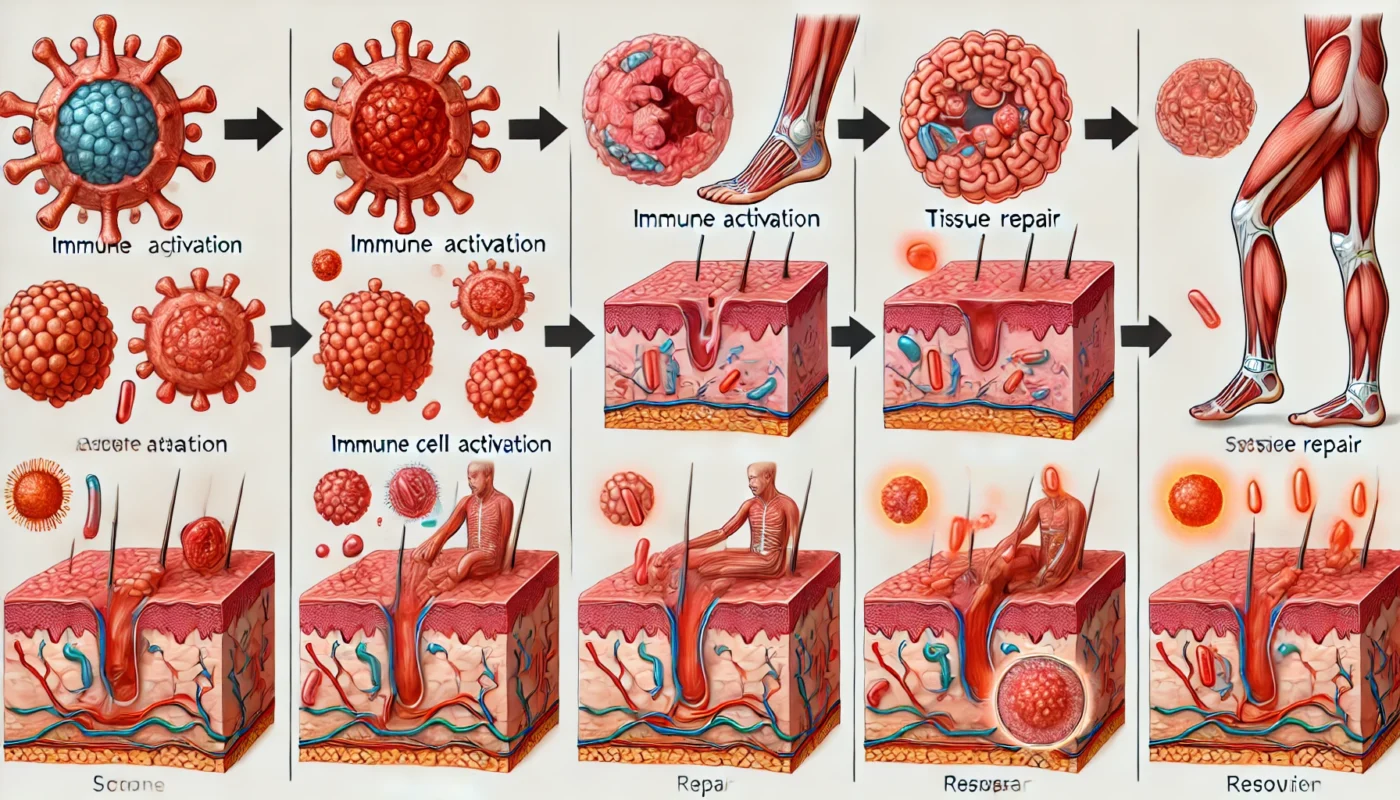
The Phases of Inflammation
The inflammatory response can be divided into three key stages: initiation, amplification, and resolution. Each phase plays a vital role in the body’s ability to heal itself.
1. Initiation Phase
The initiation phase is the first stage of inflammation and begins immediately after the body detects an injury or infection. This phase is characterized by the activation of the immune system, which includes the release of inflammatory mediators, such as histamines, cytokines, and prostaglandins.
Activation of Immune System
Upon detecting injury, the immune system springs into action. The initial response involves cells like mast cells releasing histamines, which trigger vasodilation and increased blood flow to the area. This is what causes the redness and warmth associated with inflammation.
Other immune cells, such as dendritic cells and macrophages, recognize pathogens or damage-associated signals and release cytokines. These signaling molecules coordinate the immune response, attracting more immune cells to the site of injury.
Role of Inflammatory Mediators
Inflammatory mediators are crucial in orchestrating the body’s response to injury. Histamines cause blood vessels to become more permeable, allowing immune cells to access the affected tissue. Prostaglandins contribute to pain and fever, which are protective responses that limit movement and allow healing.
These mediators also activate the complement system, a series of proteins that enhance the ability of immune cells to clear pathogens. The complement system is essential for marking pathogens for destruction and clearing out debris from damaged cells.
Setting the Stage for Healing
The initiation phase sets the groundwork for healing by assembling the necessary cellular components and mediators. By increasing blood flow and permeability, it ensures that immune cells can reach the site of injury quickly. This rapid response is critical for preventing the spread of infection and minimizing tissue damage.
The body’s focus during this phase is to isolate the threat and begin the process of removing harmful agents. This stage is self-limiting, with feedback mechanisms in place to transition to the next phase once the initial response is complete.
2. Amplification Phase
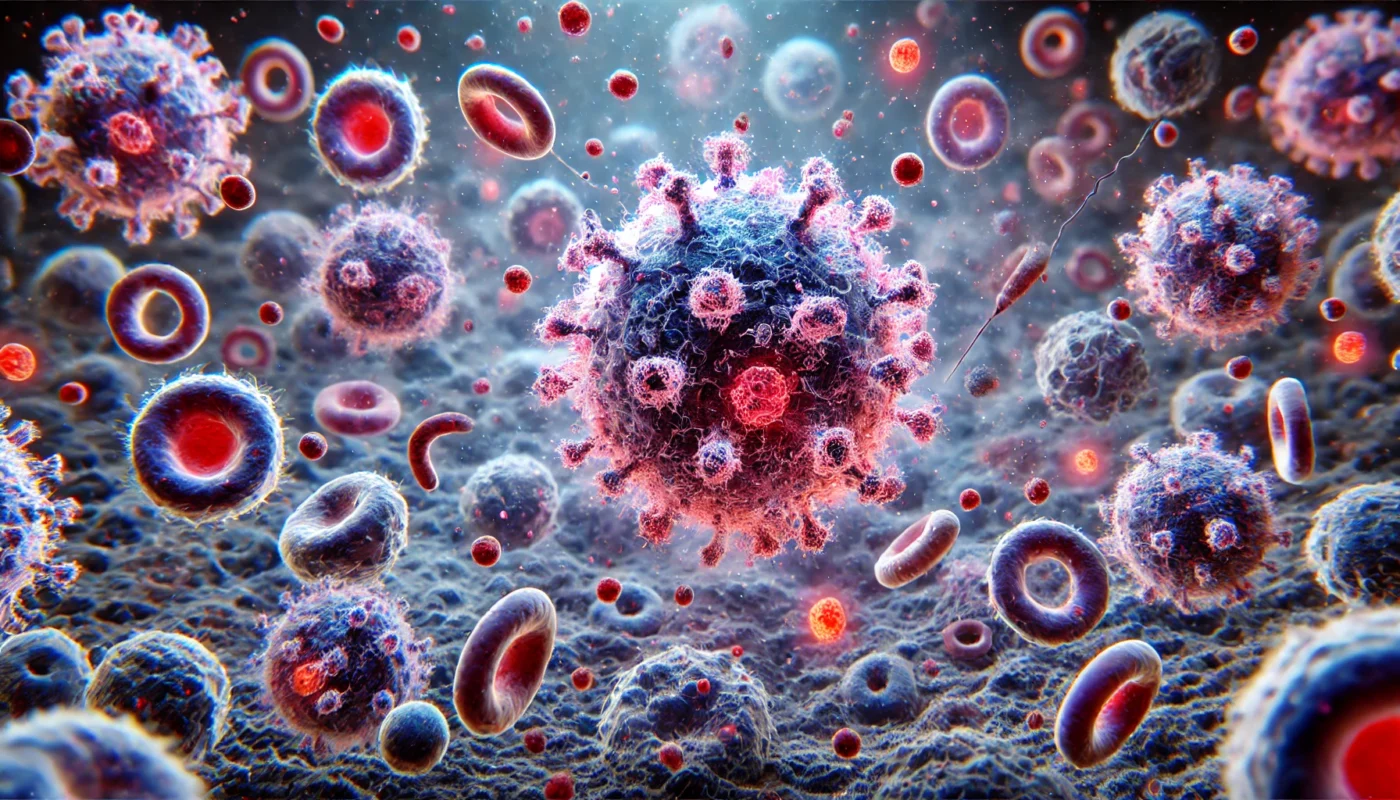
The amplification phase is the second stage of inflammation and involves the recruitment and activation of additional immune cells. This phase is characterized by the release of more inflammatory mediators, which further increase blood flow and vascular permeability.
Recruitment of Immune Cells
The primary goal of the amplification phase is to bolster the body’s defensive line. Chemotactic signals guide additional immune cells, such as neutrophils and macrophages, to the site of injury. These cells are essential for engulfing pathogens and debris, a process known as phagocytosis.
Neutrophils, being the first responders, play a crucial role in containing the infection. They release enzymes and reactive oxygen species to destroy pathogens. Macrophages follow, clearing out dead cells and further stimulating the immune response if needed.
Enhanced Immune Response
The amplification phase intensifies the immune response, ensuring that the threat is adequately contained. This phase is marked by a feedback loop where immune cells release more cytokines, attracting even more cells to the area. The heightened response is vital for overwhelming the infectious agents and preventing their spread.
The body’s ability to escalate the immune response quickly is essential for effective healing. By concentrating immune activity at the site of injury, the body minimizes the risk of systemic infection and maximizes the efficiency of pathogen clearance.
Containment and Elimination
The culmination of the amplification phase is the containment and elimination of the initial threat. Phagocytic cells remove pathogens and debris, while other immune cells produce antibodies to neutralize invaders. This concentrated effort ensures that the inflammatory response remains localized, preventing unnecessary tissue damage.
The phase sets the stage for tissue repair by clearing the area of harmful substances. Once the threat is neutralized, the body begins transitioning to the resolution phase, focusing on restoring normal tissue function and structure.
3. Resolution Phase
The resolution phase is the final stage of inflammation and involves the restoration of tissue homeostasis. During this phase, the body begins to downregulate the inflammatory response, reducing the production of inflammatory mediators and promoting the clearance of immune cells from the site of injury.
Downregulation of Inflammation
As the need for a heightened immune response diminishes, the body shifts focus to resolving inflammation. Anti-inflammatory mediators, such as lipoxins and resolvins, are produced to counteract the effects of pro-inflammatory mediators. This helps to taper off the immune response, preventing unnecessary tissue damage.
The downregulation process involves complex signaling pathways that ensure a smooth transition from active inflammation to healing. Feedback mechanisms play a crucial role in modulating the immune response, ensuring it is neither too aggressive nor too weak.
Clearance of Immune Cells
Once the threat is neutralized, immune cells are systematically cleared from the site of injury. Macrophages play a dual role by engulfing spent immune cells and debris, facilitating the cleaning process. This clearance is essential for preventing chronic inflammation, which can occur if immune cells linger and continue to release mediators.
The body also initiates tissue repair processes, involving fibroblasts and other cells that rebuild the extracellular matrix. This is critical for restoring the integrity and function of the affected tissues, ensuring a return to normalcy.
Promotion of Tissue Repair
The resolution phase focuses on repairing and regenerating damaged tissues. Growth factors and cytokines stimulate cell proliferation and differentiation, aiding in the reconstruction of tissue architecture. This phase is crucial for restoring the function and appearance of the affected area.
By promoting tissue repair, the resolution phase ensures that healing is complete and effective. It prevents the formation of scar tissue and other abnormalities that can arise from incomplete resolution. A successful resolution phase is key to maintaining overall health and preventing chronic inflammatory conditions.

The Role of Diet and Lifestyle in Inflammation
Diet and lifestyle play a significant role in modulating the inflammatory response. Consuming a diet rich in anti-inflammatory foods, such as fruits, vegetables, whole grains, and healthy fats, can help reduce inflammation and promote healing. Conversely, a diet high in processed foods, sugar, and unhealthy fats can exacerbate inflammation and increase the risk of chronic diseases.
Anti-Inflammatory Foods
Incorporating anti-inflammatory foods into one’s diet can significantly reduce inflammation. Foods rich in omega-3 fatty acids, such as fatty fish, flaxseeds, and walnuts, are known for their anti-inflammatory properties. Antioxidant-rich fruits and vegetables, such as berries, leafy greens, and tomatoes, help combat oxidative stress, a key driver of inflammation.
Spices like turmeric and ginger contain compounds that inhibit inflammatory pathways. Including these foods regularly in the diet can help maintain a balanced inflammatory response, promoting health and well-being.
The Impact of Processed Foods
Processed foods, high in sugars, unhealthy fats, and additives, can trigger and sustain inflammation. These foods often lead to an imbalance of fatty acids, promoting the production of pro-inflammatory mediators. Moreover, they can contribute to obesity, a condition associated with chronic inflammation.
Reducing the intake of processed foods and sugars is essential for managing inflammation. By opting for whole, unprocessed foods, individuals can support their body’s natural ability to regulate inflammation effectively.
Lifestyle Factors and Inflammation
Lifestyle choices, including physical activity and stress management, have a profound impact on inflammation. Regular exercise is known to reduce the levels of inflammatory mediators and improve immune function. Activities such as brisk walking, swimming, and yoga can help maintain a healthy inflammatory response.
Stress management is equally important, as chronic stress can lead to sustained inflammation. Techniques like meditation, deep breathing, and mindfulness can reduce stress levels, supporting a balanced immune system. By prioritizing these lifestyle factors, individuals can enhance their body’s ability to manage inflammation.
Holistic and Alternative Approaches to Inflammation
Holistic and alternative approaches can complement traditional medical treatments in managing inflammation. Some popular methods include:
Herbal Remedies
Certain herbs, such as turmeric, ginger, and boswellia, have been shown to possess anti-inflammatory properties. These herbs can be incorporated into the diet or taken as supplements to help reduce inflammation.
Turmeric and Curcumin
Turmeric, a golden spice commonly used in Indian cuisine, contains curcumin, a compound with potent anti-inflammatory effects. Curcumin inhibits inflammatory pathways and reduces the production of cytokines. It can be consumed as a spice, tea, or supplement, providing a natural way to manage inflammation.
Research has shown that curcumin’s bioavailability can be enhanced by pairing it with black pepper, which contains piperine. This combination maximizes curcumin’s therapeutic potential, making it an effective tool in reducing inflammation and pain.
Ginger’s Therapeutic Effects
Ginger is another powerful anti-inflammatory herb, known for its ability to reduce pain and swelling. It contains gingerol, a compound that inhibits the production of inflammatory mediators. Ginger can be consumed fresh, dried, or as a supplement, providing versatile options for dietary inclusion.
Ginger’s effects extend beyond inflammation, offering additional benefits for digestion and immune support. Regular consumption can aid in maintaining a balanced inflammatory response, promoting overall health and wellness.
Boswellia and Joint Health
Boswellia, also known as Indian frankincense, is renowned for its anti-inflammatory properties, particularly in joint health. It works by inhibiting the production of leukotrienes, inflammatory molecules that contribute to arthritis and other inflammatory conditions. Boswellia supplements can provide relief from joint pain and stiffness, supporting mobility and quality of life.
When used consistently, boswellia can enhance the effects of other anti-inflammatory strategies, offering a holistic approach to managing inflammation. It’s important to consult a healthcare provider before beginning any new supplement regimen to ensure safety and efficacy.
Acupuncture
Acupuncture is an ancient Chinese practice that involves inserting thin needles into specific points on the body. It has been shown to modulate the immune system and reduce inflammation, making it a valuable tool for managing inflammatory conditions.
Mechanisms of Action
Acupuncture is believed to work by stimulating specific points on the body, known as acupoints, to influence physiological functions. This stimulation is thought to activate the nervous system, releasing neurotransmitters and hormones that reduce inflammation and pain.
By modulating the immune response, acupuncture can help balance pro-inflammatory and anti-inflammatory mediators. This regulation aids in reducing chronic inflammation, offering relief for conditions like arthritis and autoimmune disorders.
Evidence for Inflammatory Conditions
Research supports acupuncture’s effectiveness in managing various inflammatory conditions, including osteoarthritis, rheumatoid arthritis, and inflammatory bowel disease. Studies have shown that acupuncture can reduce pain, improve joint function, and enhance quality of life in affected individuals.
Acupuncture is often used alongside conventional treatments, providing a complementary approach that enhances overall therapeutic outcomes. Its non-invasive nature and minimal side effects make it an attractive option for many seeking alternative therapies.
Integrating Acupuncture into Treatment Plans
For those interested in incorporating acupuncture into their treatment regimen, it is essential to consult with a certified practitioner. A personalized approach, tailored to the individual’s specific needs and conditions, ensures the best possible outcomes.
When combined with dietary and lifestyle modifications, acupuncture can form part of a comprehensive strategy to manage inflammation. Regular sessions, combined with other holistic practices, can significantly improve health and well-being.
Mind-Body Practices
Mind-body practices, such as yoga, tai chi, and qigong, can help reduce stress and promote relaxation, which may, in turn, reduce inflammation. These practices emphasize the connection between the mind and body, promoting overall health and well-being.
The Role of Yoga
Yoga combines physical postures, breathing exercises, and meditation to promote physical and mental well-being. It has been shown to reduce stress hormones, which can contribute to inflammation. Regular practice can improve flexibility, strength, and overall immune function.
By fostering a sense of relaxation and mindfulness, yoga helps regulate the body’s stress response, reducing chronic inflammation. It is accessible to people of all ages and fitness levels, making it a versatile tool for managing health.
Tai Chi and Qigong for Balance
Tai chi and qigong are ancient Chinese practices that focus on slow, deliberate movements and breath control. These practices enhance balance, coordination, and relaxation, contributing to reduced stress and inflammation.
Research indicates that regular practice can improve cardiovascular health, joint function, and immune system regulation. By promoting a state of calm and focus, tai chi and qigong offer a holistic approach to managing inflammation and improving quality of life.
Incorporating Mind-Body Practices
Incorporating mind-body practices into daily routines can provide significant benefits for managing inflammation. Starting with short, regular sessions can help individuals gradually build strength and flexibility while reducing stress.
These practices can be easily integrated with other lifestyle changes, such as diet and exercise, to form a comprehensive strategy for health management. With consistent practice, individuals can experience enhanced well-being and reduced inflammatory symptoms.
Conclusion
Understanding the stages of inflammation is crucial for anyone looking to optimize their health and well-being. By recognizing the role of inflammation in the body’s healing process, individuals can make informed decisions about their diet, lifestyle, and treatment options. Incorporating holistic and alternative approaches can provide additional support in managing inflammation and promoting overall health.
Balancing Inflammation for Health
While inflammation is a natural and necessary process, it is essential to maintain a balance to prevent chronic inflammation and its associated health risks. This balance involves understanding the triggers and regulators of inflammation, enabling individuals to tailor their health strategies effectively.
By adopting a comprehensive approach that includes both traditional and alternative methods, individuals can effectively manage inflammation and improve their overall quality of life. This approach empowers individuals to take charge of their health, fostering resilience and vitality.
The Path Forward
The path to managing inflammation involves a multi-faceted approach that considers diet, lifestyle, and holistic practices. By integrating these elements, individuals can create a personalized strategy that addresses their unique needs and challenges.
As research continues to uncover the complexities of inflammation, staying informed and adaptable is key. By remaining open to new insights and approaches, individuals can enhance their ability to manage inflammation and achieve lasting health and wellness.
Empowering Health Through Knowledge
Knowledge is a powerful tool in managing inflammation and promoting health. By understanding the intricacies of the inflammatory process, individuals can make informed choices that support their well-being.
This understanding extends beyond individual health, influencing public health strategies and policies that aim to reduce the burden of inflammation-related diseases. By advocating for a holistic understanding of health, society can move towards a future where well-being is accessible to all.
Further Reading:
What Are the Five Stages of Inflammation?
Holistic health, alternative medicine, inflammation management, herbal remedies, turmeric, curcumin, ginger, boswellia, acupuncture, mind-body practices, yoga, tai chi, qigong, immune support, chronic inflammation, wellness strategies, health optimization, dietary supplements, pain relief, joint health
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.