CRPS is characterized by persistent and severe pain that typically affects one limb, such as an arm, leg, hand, or foot. It usually develops after an injury, surgery, stroke, or heart attack. Despite extensive research, the exact mechanisms behind CRPS are still unclear, which makes it a challenging condition to treat effectively. The pain associated with CRPS is often disproportionate to the initial injury, and patients may experience symptoms like changes in skin color and temperature, swelling, and abnormal sweating.
You may also like: Innovative Procedures for Chronic Pain Relief
Historical Background and Evolution
The understanding of CRPS has evolved significantly over the years. Initially described in the 19th century as “causalgia,” the condition was observed in soldiers who suffered limb injuries. Over time, medical research has expanded our understanding, recognizing CRPS as a complex interplay of nervous system dysfunction.

Symptoms and Diagnosis
CRPS presents a range of symptoms that can vary from person to person. Common symptoms include burning pain, sensitivity to touch, and joint stiffness. Diagnosing CRPS involves a thorough clinical examination and often ruling out other conditions. Physicians rely on patient history and symptom patterns to make an accurate diagnosis.
Theories Behind CRPS
Several theories attempt to explain CRPS, though none are definitive. One theory suggests an abnormal response of the immune system, while another proposes dysfunction in the sympathetic nervous system. These hypotheses guide ongoing research and influence treatment approaches, though more studies are needed to fully understand the condition’s root causes.
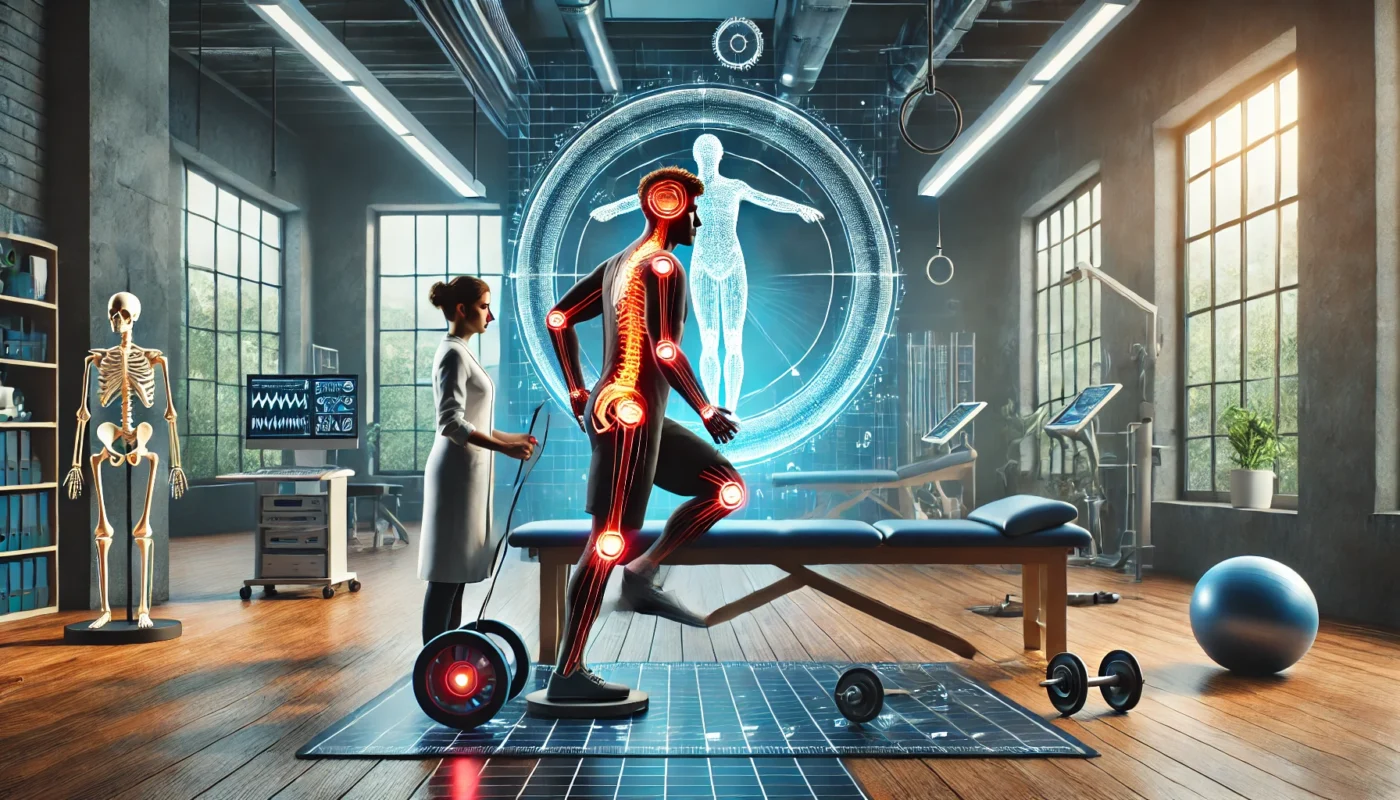
The Importance of Physical Therapy in CRPS Treatment
Physical therapy is widely recognized as a cornerstone in the treatment of CRPS. It plays a crucial role not only in pain management but also in restoring movement and function. Physical therapists are specially trained to help patients with CRPS by designing individualized treatment plans that address their unique needs and conditions.
Goals of Physical Therapy in CRPS
The primary objectives of physical therapy for CRPS include:
- Pain Reduction: Through various techniques and exercises, physical therapy aims to alleviate pain and discomfort. Techniques such as manual therapy, TENS, and gentle stretching are used to target pain pathways and reduce discomfort.
- Improved Mobility: Enhancing the range of motion in the affected limb is vital to regaining normal function. Therapists may employ stretching exercises and mobilization techniques to prevent stiffness and improve flexibility.
- Strength Building: Strengthening exercises help restore muscle function and prevent atrophy. Resistance training and weight-bearing exercises are introduced gradually to build muscle endurance without exacerbating pain.
- Normalization of Sensation: Techniques to desensitize the affected limb can reduce pain and sensitivity. Sensory re-education and exposure to varying textures help recalibrate the nervous system’s response to stimuli.
Comprehensive Assessment and Personalized Plans
Each CRPS case is unique, requiring a tailored approach. Physical therapists conduct comprehensive assessments to evaluate pain levels, mobility, and functional limitations. This information is crucial in developing a personalized treatment plan that aligns with the patient’s goals and lifestyle.
Interdisciplinary Collaboration
Successful CRPS management often involves a multidisciplinary team. Physical therapists collaborate with doctors, occupational therapists, and psychologists to ensure a holistic approach. This collaboration enhances the treatment’s effectiveness and addresses both physical and psychological aspects of CRPS.
Key Physical Therapy Techniques for CRPS
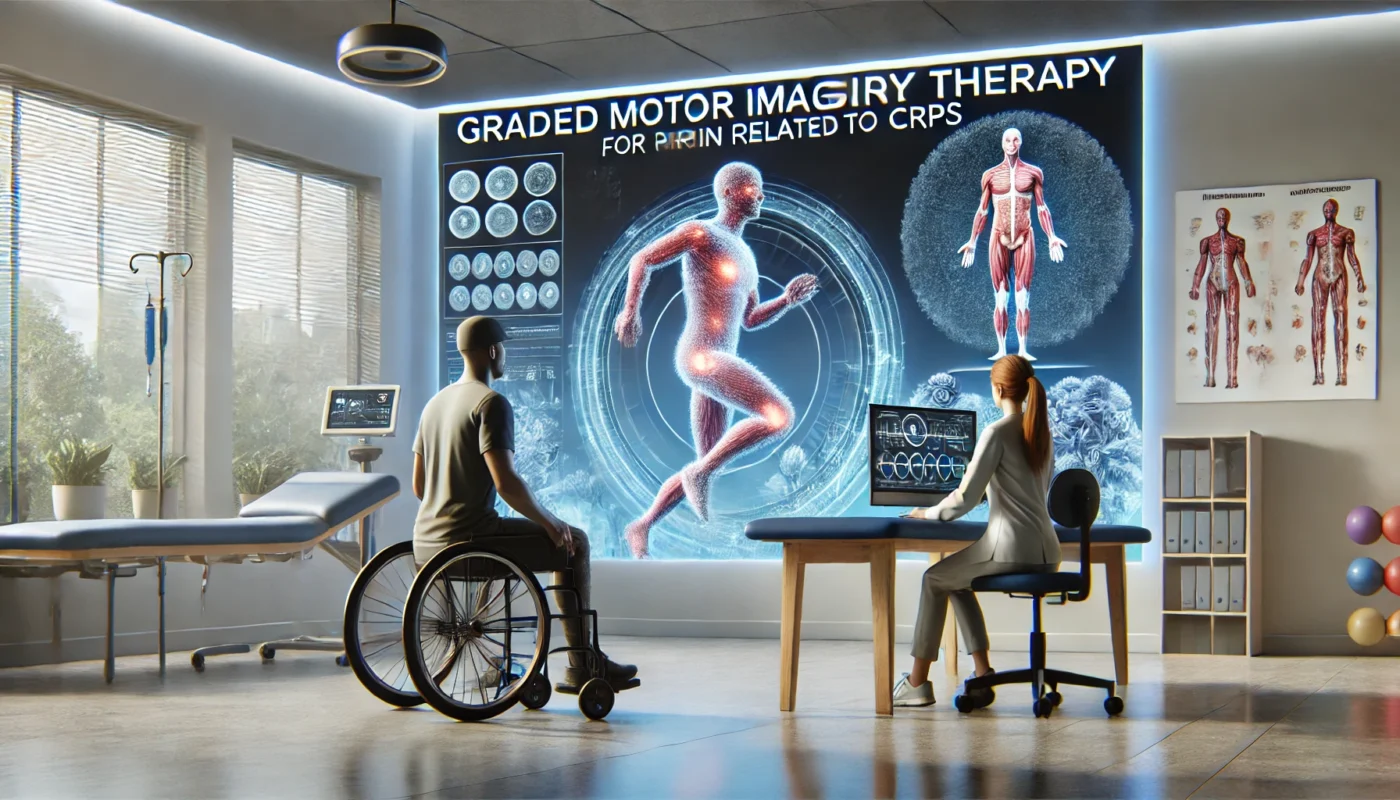
Graded Motor Imagery
Graded Motor Imagery (GMI) is a cutting-edge technique that involves a series of mental and physical exercises designed to retrain the brain’s perception of the affected limb. This approach can help reduce pain and improve movement by gradually altering the brain’s response to the limb.
- Phase 1: Laterality Reconstruction: Patients begin by distinguishing between images of left and right limbs. This phase reestablishes neural pathways without physical movement.
- Phase 2: Imagined Movements: Patients visualize moving the affected limb without actual movement. This mental exercise stimulates the brain and prepares it for physical activities.
- Phase 3: Mirror Therapy: Mirrors are used to create the illusion of movement, further enhancing neural plasticity and reducing pain perception.
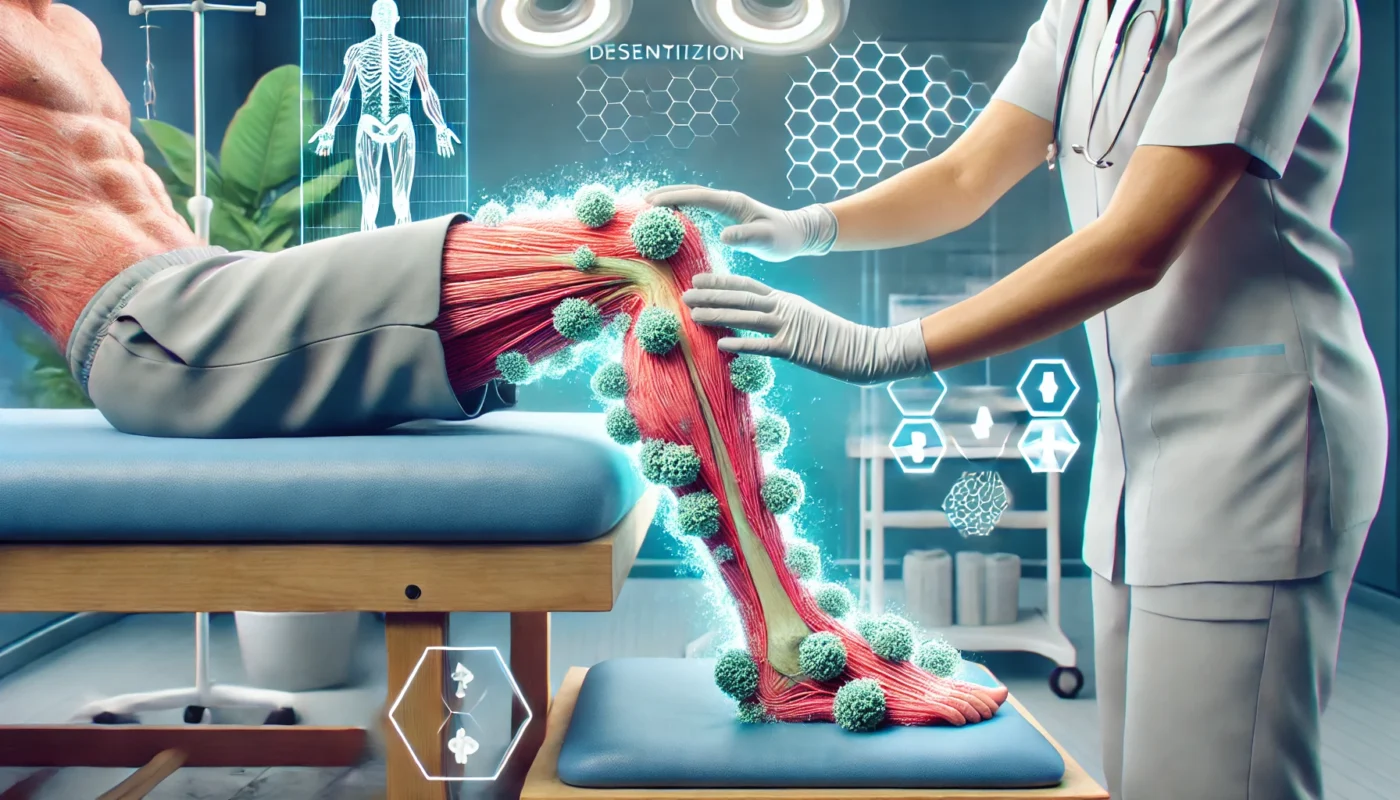
Desensitization
Desensitization techniques are employed to help patients gradually become accustomed to touching or moving the affected area. By introducing different textures and stimuli, these methods can help reduce hypersensitivity and pain.
- Texture Introduction: Gradual exposure to various textures, such as soft fabrics or rough surfaces, helps decrease sensitivity. This process retrains the sensory nerves to tolerate normal tactile input.
- Pressure Application: Controlled pressure is applied using hands or tools to desensitize the area. This technique helps reduce pain associated with touch and pressure.
- Temperature Variation: Alternating warm and cool stimuli can aid in normalizing temperature sensitivity. It also helps in reducing autonomic dysregulation in the affected limb.
Mirror Therapy
Mirror therapy involves using a mirror to reflect the unaffected limb, creating the illusion that the affected limb is moving without pain. This visual trick can help rewire the brain’s perception of pain and improve motor function.
- Setup and Execution: A mirror is placed perpendicular to the patient’s body, reflecting the unaffected limb. The patient performs movements with the unaffected limb while watching the reflection.
- Cognitive Engagement: The brain is tricked into perceiving movement in the affected limb, which can help reduce pain and improve mobility over time.
- Routine Integration: Consistent practice is key to maximizing the benefits of mirror therapy. Sessions are typically short but frequent, reinforcing the brain’s new perception pathways.
Aquatic Therapy
Aquatic therapy offers a low-impact environment where patients can perform exercises without the burden of gravity. The water’s buoyancy supports the body, allowing for improved movement and reduced pain.
- Benefits of Buoyancy: Water supports the body, reducing strain on joints and muscles. This allows patients to perform exercises they might not be able to do on land.
- Resistance and Flexibility: Water provides natural resistance, helping to build strength and flexibility. Exercises are tailored to each patient’s capabilities and progress over time.
- Therapeutic Environment: The calming nature of water can also have psychological benefits, reducing stress and anxiety associated with CRPS.
Manual Therapy
Physical therapists may use hands-on techniques such as massage and joint mobilization to enhance mobility and decrease pain. These methods can alleviate muscle tension and improve circulation in the affected area.
- Massage Techniques: Gentle massage helps relax muscles, improve circulation, and reduce swelling. It can also provide temporary pain relief.
- Joint Mobilization: Techniques to mobilize stiff joints can restore range of motion and improve function. Therapists use specific movements to target joint capsules and surrounding tissues.
- Fascial Release: Myofascial release techniques address restrictions in the fascia, the connective tissue surrounding muscles. This can alleviate pain and improve mobility.
Practical Tips for Managing CRPS with Physical Therapy
Consistency is Key
Regular physical therapy sessions are crucial for making progress. Adhering to the therapist’s recommendations and performing exercises at home can significantly impact recovery.
- Creating a Routine: Establishing a consistent schedule for therapy sessions and home exercises helps reinforce progress. Consistency ensures that therapeutic benefits are sustained over time.
- Tracking Progress: Keeping a journal of symptoms, exercises, and improvements can motivate patients and provide valuable feedback for therapists. This record helps in adjusting the treatment plan as needed.
- Adapting to Changes: Being flexible with the routine is essential, especially when experiencing fluctuations in pain or mobility. Therapists can provide alternative exercises to accommodate these changes.
Communication with Your Therapist
Open communication with your physical therapist is essential. Discuss your symptoms, concerns, and progress to ensure that the treatment plan remains effective and personalized.
- Feedback Loop: Sharing detailed feedback about what is and isn’t working helps therapists tailor the program more effectively. Open dialogue fosters a collaborative approach to treatment.
- Goal Setting: Establishing short-term and long-term goals with the therapist provides direction and motivation. These goals should be realistic and aligned with the patient’s lifestyle and needs.
- Expressing Concerns: Patients should feel comfortable expressing any concerns, whether they’re about pain levels, therapy techniques, or emotional well-being. This ensures the treatment plan remains supportive and effective.
Patience and Persistence
CRPS is a complex condition, and progress may be slow. Patience and persistence are vital in managing the symptoms and improving quality of life.
- Understanding the Timeline: Recovery from CRPS is not linear, and setbacks may occur. Understanding this helps manage expectations and maintain a positive outlook.
- Celebrating Small Wins: Acknowledging small improvements, such as reduced pain or increased mobility, can boost morale and encourage continued effort.
- Building Resilience: Developing coping strategies and resilience can help patients navigate the emotional and physical challenges of CRPS. Support groups or counseling may be beneficial.
Incorporating Mind-Body Techniques
In addition to physical therapy, consider incorporating mind-body techniques such as meditation, yoga, or tai chi. These practices can help reduce stress and improve overall well-being, complementing the physical therapy regimen.
- Meditation and Relaxation: Techniques such as mindfulness meditation can help reduce stress and anxiety, which can exacerbate CRPS symptoms. Regular practice promotes a sense of calm and control.
- Yoga and Tai Chi: These practices combine gentle movement with breath control and mindfulness, improving flexibility, balance, and mental clarity. They provide a holistic approach to managing pain and enhancing well-being.
- Breathing Exercises: Simple breathing techniques can be effective in managing pain and stress. Deep, rhythmic breathing helps calm the nervous system and can be practiced anywhere, anytime.
Conclusion
The journey to managing CRPS is challenging, yet physical therapy provides a valuable avenue for relief and recovery. By focusing on pain reduction, improved mobility, and strength building, physical therapy can empower individuals with CRPS to regain control over their lives. As research continues to uncover more about this enigmatic condition, the integration of holistic and alternative approaches alongside traditional therapy holds promise for those seeking comprehensive care.
Through understanding and utilizing the role of physical therapy, patients with CRPS can find hope and a pathway to a better quality of life. Remember, it’s important to work closely with healthcare professionals to tailor a treatment plan that meets your specific needs. With dedication and the right support, managing CRPS is within reach.
- Continued Research and Innovation: As scientific understanding of CRPS evolves, new therapies and techniques will emerge. Staying informed and open to new treatment options can enhance management strategies.
- Holistic Care Approach: Combining physical therapy with psychological support and lifestyle modifications can create a comprehensive care plan. This holistic approach addresses the multifaceted nature of CRPS.
- Empowerment through Education: Educating patients about CRPS and their treatment options empowers them to make informed decisions. Knowledge fosters self-advocacy and active participation in the recovery process.
Further Reading:
Complex Regional Pain Syndrome (CRPS)
How Can Physical Therapy Help With Complex Regional Pain Syndrome Type II (Causalgia)?
Physical Medicine and Rehabilitation for Complex Regional Pain Syndromes
physical therapy, CRPS, recovery, pain management, mind-body techniques, yoga, meditation, resilience, holistic care, patient empowerment, communication, goal setting, exercise routine, progress tracking, emotional well-being
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.

